
1
Washington State New Journeys Manual – September 2023
New Journeys Policy and Procedure Manual
Washington State New Journeys Coordinated Specialty Care

2
Washington State New Journeys Manual – September 2023
Table Of Contents
WASHINGTON STATE NEW JOURNEYS COORDINATED SPECIALTY CARE 1
INTRODUCTION TO EARLY IDENTIFICATION AND INTERVENTION FOR PSYCHOSIS 3
CHAPTER 1: NEW JOURNEYS TEAM MEMBER GUIDE 4
CHAPTER 2: RATIONALE FOR TREATING FEP WITH COORDINATED SPECIALTY CARE
(CSC) 9
CHAPTER 3: HISTORY OF NEW JOURNEYS IN WASHINGTON STATE 13
CHAPTER 4: CONCEPTUAL FRAMEWORK 17
CHAPTER 5: CORE COMPETENCIES OF NEW JOURNEYS TEAM MEMBERS 23
CHAPTER 6: FUNDING, SERVICE ARRAY, AND CODING 31
CHAPTER 7: ADMINISTRATIVE SUPPORT GUIDE 34
CHAPTER 8: STARTUP AND CASE BUILDING 37
CHAPTER 9: TEAM PROCESSES 42
CHAPTER 10: MEASUREMENT-BASED CARE AND EVALUATION 44
CHAPTER 11: REDCAP ONBOARDING 51
CHAPTER 12: REFERRAL, SCREENING, & ADMISSION 54
CHAPTER 13: ACTIVE PHASE: TIMING OF ENGAGEMENT & PROVISION OF NEW JOURNEYS
INTERVENTIONS 58
CHAPTER 14: MAINTENANCE AND DISCHARGE PHASES OF TREATMENT 63
REFERENCES 65
GLOSSARY OF TERMS 69
APPENDIX A: EXAMPLE JOB DESCRIPTIONS 73
APPENDIX B: RECURRING TRAINING AND CONSULTATION HOURS FOR NEW JOURNEYS
TEAM MEMBERS 82
APPENDIX C: EXAMPLE OF AGENCY LEVEL NEW JOURNEY’S FLOW SHEET 83
APPENDIX D: EXAMPLE COMMUNITY PRESENTATION 86
APPENDIX E: NEW JOURNEYS REFERRAL FORM 94
APPENDIX F: WEEKLY TEAM MEETING PARTICIPANT TRACKING SHEET 96
APPENDIX G: NETWORK CONTACTS 98
3
Washington State New Journeys Manual – September 2023
Introduction to Early Identification and Intervention for Psychosis
SPECIAL THANKS
This manual was created in collaboration with the Washington State Health Care Authority (HCA), University of
Washington (UW), Washington State University (WSU), and various New Journeys team members throughout the state.
A special thank you to Becky Daughtry, Maria Monroe-DeVita, Dawn Miller, Katherine LaBranche, Oladunni Oluwoye,
Cammie Perretta, Jennifer Peterson, Amber Ranney, Lauren Renard, Khairul Siddiqi, Mackenzie Tennison, Shelby Terry,
and John Throckmorton for their contributions to the ongoing improvement and advancement of this manual through
monthly workgroup meetings.
PURPOSE & GOALS OF THIS MANUAL
The purpose of this manual is to provide guidelines to ensure consistency in the goals, principles, and delivery of New
Journeys services across Washington State.
This manual is a living document and will be reviewed and revised at least annually. The most current version of this
document will be available on the Health Care Authority (HCA) New Journeys and first episode psychosis webpage and
may also be accessed on the New Journeys Website.
New Journeys is an adaptation of NAVIGATE, an evidenced based practice for early intervention of psychosis. New
Journeys promotes rapid referral and treatment of symptoms of psychosis soon after they appear. Studies show that early
intervention for psychosis can change the trajectory of the illness, resulting in a decreased duration of untreated psychosis,
reduced need for inpatient hospitalization, improved social and vocational outcomes, a decreased risk of subsequent
episodes, and ultimately a decreased risk of long-term disability associated with Schizophrenia Spectrum disorders (Kane
et al., 2016).
The broad vision of New Journeys in Washington State is to:
(1) Make screening for early psychosis among youth and young adults a universal health practice
(2) Ensure availability of evidence-based health and recovery support interventions to those in need, with the ultimate
objective of decreasing the duration of untreated psychosis (DUP)
(3) Improve the quality of life for individuals experiencing early psychosis and their families
Note on the use of the word “program”
For the purposes of this manual, the word “program” is used to refer to the implementation of the New Journeys Model by
a New Journeys team.
4
Washington State New Journeys Manual – September 2023
CHAPTER 1: NEW JOURNEYS TEAM MEMBER GUIDE
1
Welcome to New Journeys! New Journeys is a collaboration between HCA, UW, WSU, and various behavioral health
agencies throughout the state of Washington. New Journeys is based on NAVIGATE, an evidenced-based Coordinated
Specialty Care (CSC) model for youth and young adults ages of 15-40 who are experiencing first episode psychosis
(FEP). The primary focus of the model is strategic community outreach and education about FEP as well as targeted
program recruitment to decrease DUP in the community in which the team serves. Each New Journeys team serves no
more than 30 individuals, at any given time, and teams are expected to provide services wherever an individual is most
comfortable, including in home, community, and clinic settings.
Current funding (through the Team Based Rate, TBR) allows individuals to receive treatment from New Journeys for a
maximum of 24 months. In 2022, the average duration of participation with a New Journeys team was 22 months (Elson
S. Floyd College of Medicine – Washington State University, 2022). However, teams may determine if treatment beyond
24 months is clinically appropriate and may continue to provide services using typical outpatient billing codes, once an
individual is no longer eligible for the TBR. Please see Chapter 6 for additional details.
Within New Journeys, the multi-disciplinary team members work collaboratively with the individual experiencing
psychosis, as well as their natural supports, to provide evidenced based treatment for FEP. Teams have a responsibility to
a) instill hope in individuals about their ability to recover from FEP, b) help them establish and work towards personal
meaningful goals, thereby empowering them to make progress towards the lives they want to lead and c) provide the best
treatment available for their illness.
Getting Started
To become an established, New Journeys site, potential contractors collaborate with HCA to establish funding and
become integrated into the New Journeys Network. Once a site is contracted with HCA, they enter the startup phase.
During the startup phase, team members are hired, training is completed, and internal infrastructure to support New
Journeys activities are developed. During startup phase, teams will establish an internal referral and screening process and
begin case building. Case building occurs once a team is ready to accept referrals and begin providing New Journeys
services. Teams will admit no more than three (3) individuals per month to ensures that service intensity expectations can
be met. Typically, teams require two years of case building to be considered fully performing and become an attested New
Journeys team with a full caseload (25-30 individuals enrolled). An attested provider refers to a team that has completed
start-up and is recognized by the New Journeys network as having completed the necessary training to provide New
Journeys services and is ready to accept referrals. An attestation form is completed and submitted to HCA documenting
the basic training, staffing and fidelity requirements have been met. These phases are discussed in greater detail in
Chapter 8.
One of the first tasks of a new site is to staff the multi-disciplinary team. The team consists of several different
professional specializations to support an individual in their recovery from FEP. Staffing a full New Journeys team can
take time and may require concerted recruitment efforts on behalf of the agency (example Job Descriptions can be found
in Appendix A). Agencies can share their job postings with the UW Implementation Team to be shared on the UW
SPIRIT Lab Website and with the WSU Measurement Delivery and Evaluation Team to be shared on the New Journeys
Website.
1
Parts of the New Journeys Team Member Manual have been reprinted and adapted with permission from NAVIGATE Consultants
and NAVIGATE manual co-authors Susan Gingerich and Kim Mueser (2020). The original manual was written by Kim T. Mueser
and Susan Gingerich, with contributing authors (in alphabetical order): Jean Addington, Mary F. Brunette, Cori Cather, Jennifer D.
Gottlieb, David W. Lynde, and David L. Penn. The author of the revision of 2020 is Susan Gingerich.

5
Washington State New Journeys Manual – September 2023
The New Journeys team members are depicted in Figure 1. Team members include: Program Director/Family Education
Provider (1.0 FTE), Psychiatric Care Provider (0.25 FTE), Individual Resiliency Training (IRT) Therapist (1.0 FTE),
Supported Employment and Education (SEE) Specialist (1.0 FTE), Peer Support Specialist (0.5 FTE), Case Manager
and/or Registered Nurse Care Manager (0.5 FTE)
2
. Variations in this staffing model should be approved by HCA and the
UW implementation team. More information on each role can be found in Chapter 5.
Figure 1. FTE for New Journeys Team Members
Eligibility Criteria
New Journeys is a treatment match model, which means that not everyone who is referred to a New Journeys will be
eligible for services. A primary role of each team’s Program Director is to complete appropriate screening, including
differential diagnosis for each referral that is received. This in-depth screening process becomes a vital service to the
community and ensures individuals being referred receive services that best meet their individual needs. Referral,
Screening, and Admission are discussed in greater detail in Chapter 12 of this manual. Teams screen referrals for
eligibility using the eligibility criteria outlined in Table 1.
2
Teams may choose to substitute a nurse care manager (~0.2 FTE) for all or part of the case manager FTE count.
6
Washington State New Journeys Manual – September 2023
Table 1. New Journeys Eligibility Criteria
Performance Indicators
There are many differences between New Journeys and regular outpatient care. As discussed previously, New Journeys is
an evidenced based practice that provides a multi-disciplinary approach to care. As such, case load sizes are lower and
additional time is needed for activities such as differential diagnosis of referrals, training and consultation (beyond
licensing and agency requirements), fidelity review activities, outreach and education to the community about FEP, etc.
The low caseloads, additional support from other team members, and ongoing training make New Journeys a desirable
model to be a part of. As teams are starting up, it is important bring awareness to several areas of performance for New
Journeys teams. They are divided into the following categories, which are outlined in Table 2 below: Participant services,
staff training and consultation, cross-systems collaboration, funding and sustainability, communications, and fidelity
monitoring.
3
The NAVIGATE model is not suited to provide treatment to those experiencing co-morbid intellectual disability with an IQ below
70. This is due to the likely need for ongoing, intensive supports that are above and beyond what NAVIGATE/New Journeys is able to
provide but can be provided within the Developmental Disabilities system. Program Directors are not responsible for assessing an
individual’s IQ but should be aware of this eligibility criterion when gathering collateral information and records during the screening
process.
4
During differential diagnosis, a Program Director should differentiate between psychotic like symptoms that are sometimes seen in
autism spectrum disorder and new and emerging symptoms of psychosis indicative of a psychotic disorder. NAVIGATE/New
Journeys does not include any training or specific interventions focused on managing the symptoms, behaviors, and cognitive
impairments associated with autism. New Journeys providers can work to determine the severity of the symptoms associated with
autism and whether or not psychosis is the primary presenting problem. The UW Implementation Team provides consultation related
to Differential Diagnosis to help assist Program Directors in these situations.
Eligibility Criteria
The psychosis is NOT known to be caused by:
1. Ages 15-40
2. Psychotic symptoms have been present between 1
week and 2 years
3. Primary diagnosis of one of the following:
• Schizophrenia
• Schizoaffective disorder
• Schizophreniform disorder
• Brief psychotic disorder
• Delusional disorder
• Other specified psychotic disorder
4. IQ over 70
3
1. Mood disorder with psychotic features
2. Pervasive developmental disorder and/or autism
spectrum disorder
4
3. Psychotic disorder due to another medical condition
including medication induced psychotic disorder
4. The temporary effects of substance use or withdraw
7
Washington State New Journeys Manual – September 2023
Table 2. Performance Indicators
Area
Goals
Interventions
Participant
Services
Meet individuals where they are at: inspire
hope and eliminate barriers to treatment that
are traditionally experienced by those
experiencing FEP. New Journeys aims to
reduce the risk of individuals dropping out of
services and works to increase their overall
quality of life.
Provide an array of Medicaid and State funded services as
outlined in the New Journeys Model. Including but not
limited to:
• Community Education and Outreach
• Screening of referrals and differential diagnosis of FEP
• Behavioral Health intake evaluations and assessments
• Individual Treatment Services
• Family Education and Treatment
• Therapeutic Psychoeducation
• Case Management
• Psychiatry/Medication Management
• Community Support Services
• Peer Support
• Supported Employment/Education (SEE)
• Other New Journey services such a psychoeducational
group and/or multifamily groups.
• Interpreter Services
Staff Training and
Consultation
Ongoing education and consultation for New
Journeys staff
Each team member should attend New Journeys specific
training, including but not limited to:
• WSU orientation and training
• UW startup training
• Monthly role specific consultation calls
• Monthly ECHO Clinics
• Monthly Differential Diagnosis call
• Pat Deegan Common Ground Academy + Library
• Other orientation and training opportunities as
identified by the UW implementation team and WSU
evaluation team
Fidelity
Monitoring
To evaluate adherence to the model, areas of
success, and identify areas for additional
support and training.
• Each New Journey team will participate in annual
Fidelity Monitoring
• Each team will utilize the New Journeys Assessment
Battery and enter data into the New Journeys data
platform
• Selected members of each New Journeys team will be
trained as peer reviewers for the fidelity review process
Funding and
Sustainability
Each agency will develop internal processes
with the agency to optimize reimbursement to
support a financially sustainable program that
is adequately supported to provide services to
fidelity.
• Administration will set up budgets, manage resources,
and maximize billing practices to support the teams to
function to fidelity of the model
• Administration will optimize braided funding sources
through contractual agreements available in their region

8
Washington State New Journeys Manual – September 2023
Using the NAVIGATE Manuals
As you are getting started, it is important to not only become familiar with the materials in this manual but also with the
NAVIGATE model of CSC from which New Journeys was developed. New Journeys uses the NAVIGATE materials,
including the NAVIGATE manuals for the following team roles and respective interventions: Program Director, Family
Education, Individual Resiliency Training (IRT), Supported Employment and Education (SEE) , and Psychiatric Care
Provider. When NAVIGATE was developed, they did not yet have a Peer Specialist or Case Manager on the team. As a
result, there is currently no Case Manager manual. New Journeys does use the Peer manual developed by OnTrackNY. A
Nurse Care Manager Manual was developed by the UW Implementation team and available to teams with Nurse Care
Managers.
The NAVIGATE manuals will familiarize team members with the background and conceptual framework of each
intervention and provide critical tools to implement each service component. No one is expected to master all the material
contained in each manual at one time. Learning for each team member takes place throughout their role; through the
implementation of the manual and materials in sessions with individuals and their natural supports, by participating in
team meetings and supervision, as well as by engaging in monthly consultation calls, ECHO Clinics, and ongoing training
with the UW Implementation Team (more information about consultation and ECHO is included in Chapter 7 and
Appendix B).
As you learn about NAVIGATE and use the interventions outlined by your role, it may be helpful to have your manual
with you during sessions and become familiar with the session guidelines, handouts, and worksheets in advance. Such
preparation helps with a mutual learning process between the clinician, the individual, and natural supports. Everyone has
something important to teach the other and the shared learning experience will be helpful to working together on the
individual’s goals.

9
Washington State New Journeys Manual – September 2023
CHAPTER 2: RATIONALE FOR TREATING FEP WITH COORDINATED
SPECIALTY CARE (CSC)
The Long-term Disability of Schizophrenia
Schizophrenia is a major mental illness characterized by psychosis, negative symptoms (e.g., apathy, social withdrawal,
anhedonia), and cognitive impairment. Depression and substance abuse commonly co-occur with schizophrenia spectrum
diagnoses. Individuals with schizophrenia spectrum disorders can have challenges in the areas of work, school, parenting,
self-care, independent living, interpersonal relationships, and leisure time.
Among adult psychiatric disorders, schizophrenia is the most disabling. Only 1% in the general population has
schizophrenia, but over 30% of all spending for mental health treatment in the U.S. in 2001 was accounted for by
schizophrenia—about $34 billion (Mark et al., 2005). The high cost of treating schizophrenia is only one dimension of the
impact of the illness, which has major effects on individuals, families, and society. The toll that schizophrenia takes,
including premature death, family caregiving, unemployment, criminal justice costs, and physical and emotional distress,
is striking (Samnaliev & Clark, 2008). According to the World Health Organization, the combined economic and social
costs of schizophrenia place it among the world’s top ten causes of disability worldwide (Murray & Lopez, 1996).
Considering the magnitude of the impact of schizophrenia, interventions designed to treat the disorder effectively at the
earliest possible point (e.g., during the first episode of psychosis) have the potential to improve individual’s long-term
trajectory, and to reduce the global burden of the illness.
Why Coordinated Specialty Care (CSC)?
On average, people may experience new psychotic symptoms for months, and sometimes even years, before receiving any
psychiatric treatment (Häfner et al., 2003; Perkins et al., 2005). There are multiple reasons an individual may delay
treatment, including the stigma of mental illness and schizophrenia, a lack of awareness of the signs of psychosis and the
resources to treat such disorders, individuals may be aware that something unusual is happening but may not know that
the changes are signs of a treatable mental illness (Corrigan, 2004; Judge et al., 2005). These factors can prevent
individuals from getting the support they need, and may result in individuals with psychosis facing houselessness,
incarceration, and isolation from natural supports due to mental illness-related behaviors (Teplin, 1994; Teplin et al.,
1996).
Even when treatment for a first episode of psychosis is successfully initiated, individuals often face challenges when the
treatment does not adequately address their specific needs and goals. Treatment may be incomplete, for example it may
include medication but no education of illness self-management skills (such as the prevention of relapses) and no skills
training for improving their functioning and quality of life. When medication is provided, non-adherence is a major
problem, which leads to increased relapse rates and increased problems with daily functioning (Robinson et al., 1999).
Research has shown that, when compared to treatment as usual, CSC can be an effective tool in addressing these issues
and helping an individual get the support they need (Kane et al., 2016).
CSC is based on models originally implemented in other countries, primarily Australia, England, New Zealand, and
Canada. CSC is considered the gold standard, evidence-based approach to delivering effective treatment for individuals
and families experiencing a first episode of psychosis. Early intervention with evidence-based treatment decreases the
DUP, improves outcomes over a lifetime, and results in reduced healthcare costs and improved quality of life for
individuals and their natural supports. The goal of CSC is to fundamentally change the trajectory and prognosis of
schizophrenia through coordinated and systematic treatment in the earliest stages of the illness (Heinssen, Goldstein, &
Azrin, 2014).
10
Washington State New Journeys Manual – September 2023
The National Institute of Mental Health (2022) defines Coordinated Specialty Care as
5
,
6
:
History of Treatment Programs for FEP
Major advances in treatment programs have been made for people with a first episode of psychosis over the last 20 years.
However, until the National Institute of Mental Health’s (NIMH) Recovery after Initial Schizophrenia Episode (RAISE)
research initiative, all of the treatment development and research on model programs for FEP occurred outside of the U.S.,
primarily in Australia, New Zealand, Europe, and Canada. For example, in an Australian treatment program (Early
Psychosis Prevention Intervention Center: EPPIC), 65 individuals were treated and followed for 8 years after initial
treatment (Mihalopoulos et al., 2009). At 8-year follow-up, people who received EPPIC treatment had decreased
symptoms, displayed fewer positive symptoms of psychosis, were more likely to be in remission, and were more likely to
be participating in employment compared to those in control groups. Additionally, the specialized EPPIC program cost
one-third as much as treatment as usual because it was more effective at reducing the long-term impacts of psychosis.
5
New Journeys has also included Peer Support and Nurse Care Management as service components to the CSC model being used
across the state
6
New Journeys considers both family members and other natural supports in implementation of the model
“a recovery-oriented, team approach to treating early psychosis that promotes easy
access to care and shared decision-making among specialists, the person experiencing
psychosis, and family members.
Specifically, coordinated specialty care involves multiple components:
Individual or group psychotherapy is tailored to a person’s recovery goals. Cognitive and
behavioral therapy focuses on developing the knowledge and skills necessary to build
resilience and cope with aspects of psychosis while maintaining and achieving personal
goals.
Family support and education programs teach family members about psychosis as well
as coping, communication, and problem-solving skills.
Medication management involves health care providers tailoring medication to a
person’s specific needs by selecting the appropriate type and dose to help reduce
psychosis symptoms.
Supported employment and education services aim to help individuals return to work or
school, using the support of a coach to help people achieve their goals.
Case management allows people with psychosis to work with a case manager to address
practical problems and improve access to needed support services.”
11
Washington State New Journeys Manual – September 2023
Limitations of Treatment Models Developed Abroad for the U.S. Context
Some of the treatment programs that were developed abroad are not feasible to implement in the U.S. for several reasons.
First, the treatment programs developed abroad have usually been offered in systems where the entire population in a
particular area is covered by a regional medical system that takes responsibility for the health of the population, allowing
for the use of fully employed teams, outreach, and public education approaches. In contrast, the U.S. has fragmented
treatment and payment systems, in which no single organization or service takes full responsibility for the treatment of
people with psychosis. Also, the comprehensive treatment models for FEP programs prior to the RAISE research initiative
had been provided in large cities that allowed for use of a full-time team. However, in the U.S., mental health services are
usually provided by local community mental health centers (CMHCs) that often serve smaller geographic catchment
areas, such that staffing a first episode program presents challenges.
Second, an important part of FEP programs developed abroad has been the use of a major public health campaign to
educate the general population about psychosis and its treatment. These campaigns have been combined with outreach and
education to people who are likely to have contact with individuals first experiencing psychotic symptoms, including
teachers, police, doctors, emergency room staff, and clergy. In the U.S., such major public education campaigns and
outreach efforts have not been a priority. In some ways, the U.S. system appeared in the past to focus more on preventing
people from entering treatment until the symptoms were so bad that treatment was unavoidable, rather than trying to
engage individuals with psychosis into treatment early in order to improve their lives and prevent long-term disability.
In summary, the NAVIGATE program (or, as our adaption is known in Washington State, New Journeys) is the result of a
response to the need to develop a program for the comprehensive treatment of people with FEP that can be implemented
and funded within the current U.S. public health care system.
NAVIGATE Outcomes
In 2008, NIMH funded two large-scale studies through the RAISE initiative. One of those studies (RAISE Early
Treatment Program – RAISE-ETP) included the first multi-site study comparing the NAVIGATE model of CSC to
Community Care (i.e., usual care) with 404 individuals in community mental health settings experiencing FEP.
Participants were assigned NAVIGATE vs. community care from 34 different agencies across 21 U.S. states. Seventeen
of these 34 mental health sites in the U.S., including urban, suburban, and rural settings, and sites serving people from
diverse ethnic and cultural backgrounds, provided NAVIGATE services
7
.
Compared to participants who received treatment as usual, NAVIGATE participants:
• Stayed in treatment longer
• Experienced more improvement in overall symptoms and quality of life
• Were more likely to receive prescriptions that conformed to best practices
• Experienced fewer medication side effects
Summary of CSC Outcomes and Cost-Effectiveness
Since the development of the NAVIGATE model in the RAISE-ETP study, studies have found that CSC programs
improve outcomes for individuals experiencing FEP. Individuals who receive treatment with a CSC team experience
significant improvements in quality of life and psychiatric symptoms. Specifically, CSC teams help reduce the impacts of
positive and negative symptoms of psychosis, depression, mood, and anxiety. In addition to impacting psychiatric
symptoms, CSC teams have positive impacts on functional outcomes, including education, employment, social and
7
To learn more about the results of the RAISE-ETP research project, you can find a list of publications up to March 2020 cited at the
end of this chapter.
12
Washington State New Journeys Manual – September 2023
interpersonal skills, and global functioning (Uzenoff et al., 2012; Brieitborde et al., 2015; Daley et al., 2020; Dixon et al.,
2015; Kane et al., 2016; Calkins et al., 2020; Kohler et al., 2020; Tanzer et al., 2021, Oluwoye et al., 2020). It should be
noted that clinical and functional outcomes can differ based that on race, ethnicity, socioeconomic status of individuals,
and DUP.
Cost-effectiveness from the initial NAVIGATE program in the RAISE-ETP study concluded that CSC programs are more
cost-effective than typical community care, with CSC program benefits exceeding costs when adjusted for Quality
Adjusted Life Years (a generic measure of disease burden; Rosenheck et al., 2016). Although CSC did not reduce the
number of individuals receiving Social Security Administration disability benefits, individuals experiencing lower
functioning and higher disability from psychosis was found to increase enrollment in disability benefits (Rosenheck et al.,
2017; Humensky et al., 2017; Smith et al., 2018). Since the initial RAISE-ETP study, CSC programs have continued to
indicate cost-effectiveness, as individuals engaged in these programs have fewer emergency room visits, hospitalizations,
and inpatient services than individuals not engaged in CSC programs (Srihari et al., 2015; Liffick et al., 2016; Murphy et
al., 2018; Nossel et al., 2018; Calkins et al., 2020).
13
Washington State New Journeys Manual – September 2023
CHAPTER 3: HISTORY OF NEW JOURNEYS IN WASHINGTON STATE
Washington State New Journeys
In 2014, Congress appropriated funds to the Substance Abuse and Mental Health Services Administration (SAMHSA) to
address the needs of individuals experiencing early serious mental illness. This grant is called the Community Mental
Health Services Block Grant (MHBG), and includes funding for all 50 states, the District of Columbia, Puerto Rico, the
U.S. Virgin Islands, and 6 Pacific jurisdictions. SAMHSA directed states to use a five percent (5%) set aside from their
portion of the MHBG to serve youth ages 15 to 25 experiencing a first episode of psychosis. In 2015, the set aside was
increased to ten percent (10%).
This funding provided the opportunity for Washington to launch New Journeys, CSC model based on NAVIGATE. New
Journeys was developed through the Division of Behavioral Health and Recovery (DBHR) partnerships with UW and
WSU to provide services to individuals experiencing FEP, curated specifically to the needs of youth and young adults
here in Washington.
After the success of the initial New Journeys Pilot site in Yakima in 2015, The Children, Youth, and Family Behavioral
Health Workgroup (CYFBWG) advocated for Second Substitute Senate Bill (2SSB) 5903. which was passed in 2019.
This legislation was accompanied by state Proviso funds that were designated for statewide expansion of New Journeys,
along with MHBG funds.
This legislation called for the creation of a Statewide Implementation Plan for evidence-based recovery supports,
development of a financing strategy for Medicaid, and statewide expansion of New Journeys based on incidence of FEP
in Washington’s population. The Statewide Implementation Plan of Coordinated Specialty Care for Early Psychosis was
prepared by the Washington Council for Behavioral Health (WCBH) and was submitted to the Legislature on January 28,
2021. This plan outlined the steps for strategic statewide implementation and strategies for funding evidence-based
recovery services for FEP.
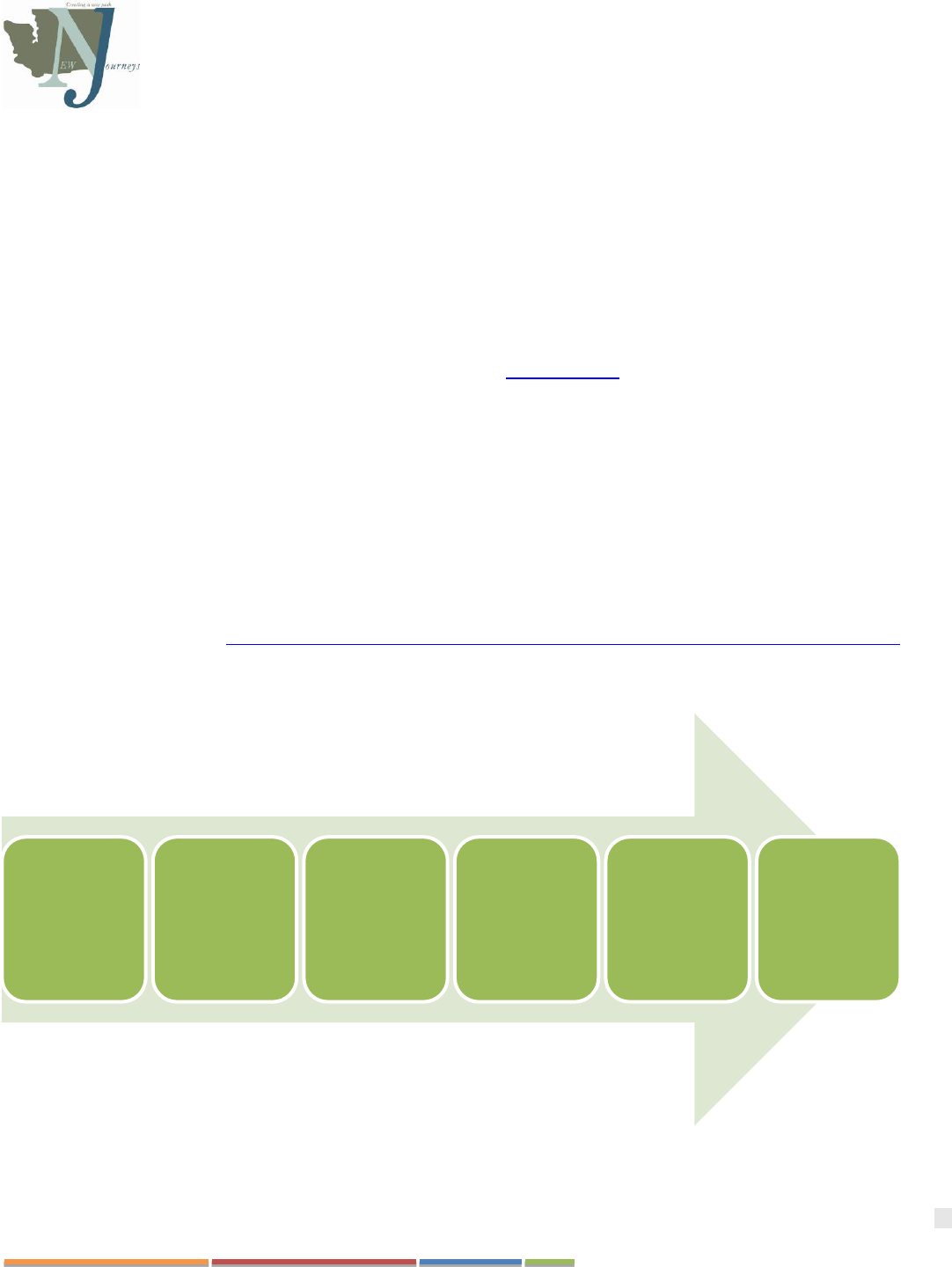
Figure 2. Timeline of Washington State New Journeys Implementation
International
research
supports
Evidenced
Based
Treatments for
FEP
2008
RAISE trials
conducted in
the U.S.
2014
U.S. Congress
directs MHBG
funds for FEP
2015
New Journeys
is piloted in
Washington
2019
2SSB 5903 is
passed into
legislation
2022
15 New
Journeys teams
statewide

14
Washington State New Journeys Manual – September 2023
Since that time, New Journeys has increased from a single team in 2015 to 11 teams in 2022. An additional four teams
launching in 2023 bringing the total to 15 teams statewide. These new teams will provide increased access in the
Spokane, Great Rivers, Salish, and North Sound regions. Continued expansion aims to provide equitable access to these
vital services throughout the state, including in geographical areas that may have reduced availability of resources.
Expansion efforts will also provide opportunities to address the unique needs that are present in the various areas of our
state, including work on adapting the model to better fit the needs of rural and Tribal communities.
Figure 3. New Journeys Team Locations as of September 2023
New Journeys Outcomes
Like NAVIGATE and other CSC models, New Journeys has also yielded many positive outcomes since this model was
implemented in Washington State in 2015 (Oluwoye et al., 2020). From 2015 to September 2022, a total of 1,189 referrals
were made to New Journeys teams across the state. Of the 1,189 referrals, 730 individuals met eligibility requirements,
and 612 received services (84%). (Elson S. Floyd School of Medicine, 2022).
The New Journeys 2022 Evaluation Report suggests that individuals who participated in New Journeys experienced
(Elson S. Floyd School of Medicine, 2022):
• A reduction in reported symptoms of psychosis
• A significant decrease in reports of depression
• A significant decrease in reports of anxiety
• A decrease in reported psychiatric hospitalizations
• Improvements in quality of life
• An increase in school enrollment from baseline at 17% to 44% after receiving services
• Attendance or procurement of at least part-time work or volunteering increased from 20% reported at enrollment to
55% post-enrollment
• Report a decrease in overall substance use since enrollment
15
Washington State New Journeys Manual – September 2023
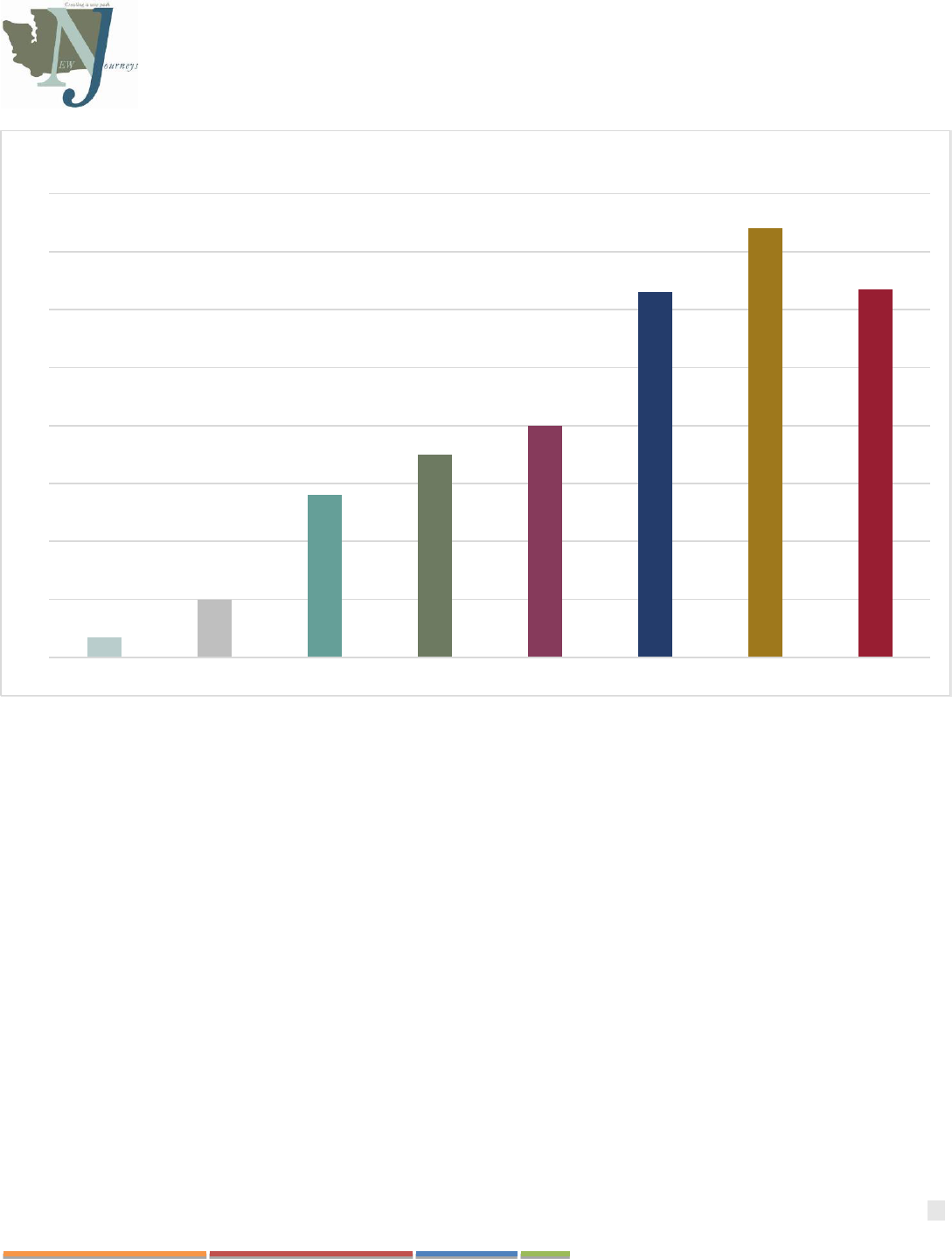
Figure 4. New Journeys Enrollment by State Fiscal Year (SFY). This figure illustrates the number of individuals who started services with New Journeys since
2015. State fiscal year falls between October 1
st
and September 30
th
; as such, the 2022 SFY as captured by this report does not include the last month of the year. Data
on enrollment date was missing for eleven individuals.
Addressing the Need in Washington State
Incidence rates of psychosis in Washington State match those across the U.S. and worldwide. In SFY 2021, Washington
State Department of Social and Health Services’ Research and Data Analysis (RDA) Division identified 4,388 Medicaid
enrollees under the age of 65 in Washington who received their first psychotic diagnosis. Among them, 1,956 were
between the ages of 15 and 40 and received at least one psychotic disorder diagnosis covered by New Journeys (Figure 5).
However, this is likely a conservative estimate of the incidence of FEP, because it does not include individuals who were
experiencing symptoms but did not encounter a Medicaid provider. This estimate only accounted for individuals enrolled
in Medicaid or dually enrolled in Medicare during two of the last three years. Individuals newly enrolled in Medicaid or
those with commercial insurance were not accounted for.
0
20
40
60
80
100
120
140
160
2015 2016 2017 2018 2019 2020 2021 2022
Number of Individuals Served by State Fiscal Year

16
Washington State New Journeys Manual – September 2023
FEP Cases Among Medicaid Enrollees
SFY 2021 TOTAL STATEWIDE = 4,388
Potential Cases Meeting New Journeys Criteria
SFY 2021 TOTAL STATEWIDE = 1,956
Figure 5. Estimated First Psychotic Diagnoses among Medicaid Enrollees by County
17
Washington State New Journeys Manual – September 2023
CHAPTER 4: CONCEPTUAL FRAMEWORK
People diagnosed with a schizophrenia spectrum disorder may experience an array of symptoms including psychotic
experiences, negative symptoms, cognitive impairment, depression, and anxiety. Psychotic symptoms may include
hallucinations, delusions, and/or disorganized thinking/behavior. Individuals may also experience prominent negative
symptoms, such as a lack of expressiveness or motivation, which are defining characteristics of schizophrenia and
schizophrenia spectrum disorders. Problems with cognitive functioning can present as confused thinking, which may
interfere with work, independent living, and social relationships (Green, 1996; McGurk & Mueser, 2004). Depression and
anxiety are also common features of schizophrenia, although they are not included in the diagnostic criteria. Depression
and/or high levels of anxiety may be the first sign of the illness before the onset of psychotic symptoms (Häfner et al.,
1999), and depression often remains one of the most persistent syndromes among people with schizophrenia (Häfner & an
der Heiden, 2008).
Due to the complexity of challenges an individual experiencing psychosis may face (including long term disability,
increased risk of hospitalization, and increased risk of homelessness. This topic is outlined in further detail in Chapter 2),
young people experiencing FEP are especially vulnerable to suicidal ideation and suicide attempts (Power, 2004).
Moreover, one-half of individuals with this illness develop substance use disorders (abuse or dependence). Overall, these
symptoms negatively impact components of an individual’s recovery and resiliency, including social/leisure functioning,
well-being, and role functioning. However, there is hope! Early detection and intervention of psychosis can fundamentally
change the trajectory of the illness. CSC teams utilize various strategies to help individuals experiencing FEP live their
life, rather than being defined by their symptoms or diagnosis. New Journeys, and the NAVIGATE model, utilized
multiple recovery-oriented frameworks outlined throughout the rest of this chapter.
Recovery and Resiliency
New perspectives on recovery and resiliency do not focus on the severity or persistence of psychiatric symptoms, rather
the focus is on a person’s ability to experience a rewarding and meaningful life. As Pat Deegan puts it, recovery
orientation is shifting the focus from “what’s the matter with you” to “what matters to you. Anthony (1993) defined
recovery as, “the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of
mental illness.” This way of thinking about recovery and resiliency is consistent with models of positive health, which
identify mental health is improved through leading a life of purpose and having quality connections with others (Ryff &
Singer, 1998). New Journeys utilizes this recovery-oriented approach that builds on an individual’s capacity for resiliency.
The President’s New Freedom Commission Report (2003) affirmed the pursuit of recovery and resiliency as an important
focus of mental health treatment. According to the Report, “Recovery is the process in which people are able to live,
work, learn, and participate fully in their communities”. The Commission also called for a transformation of the mental
health system and argued for a system level approach focusing on service recipients and their families as partners in the
mental health system. Treatment choice should be guided by shared decision-making with recovery and resiliency as the
primary goal.
New Journeys embraces this view of recovery and resiliency. Specifically, we define recovery and resiliency as:
• Social/leisure functioning (e.g., quality of social relationships, involvement in leisure activities, independent and
self-care living skills)
• Role functioning (e.g., school, work, parenting)
• Well-being (e.g., self-esteem, hope, sense of purpose, enjoyment of life)
Illness Management
Illness management approaches to treating schizophrenia derived from the stress-vulnerability model (Liberman et al.,
1986; Nuechterlein & Dawson, 1984; Zubin & Spring, 1977). Illness management helps people achieve recovery and
18
Washington State New Journeys Manual – September 2023
resiliency by teaching information about the symptoms of mental illness, helping them control their symptoms, and
helping them prevent relapses so that they are better able to pursue their personal goals.
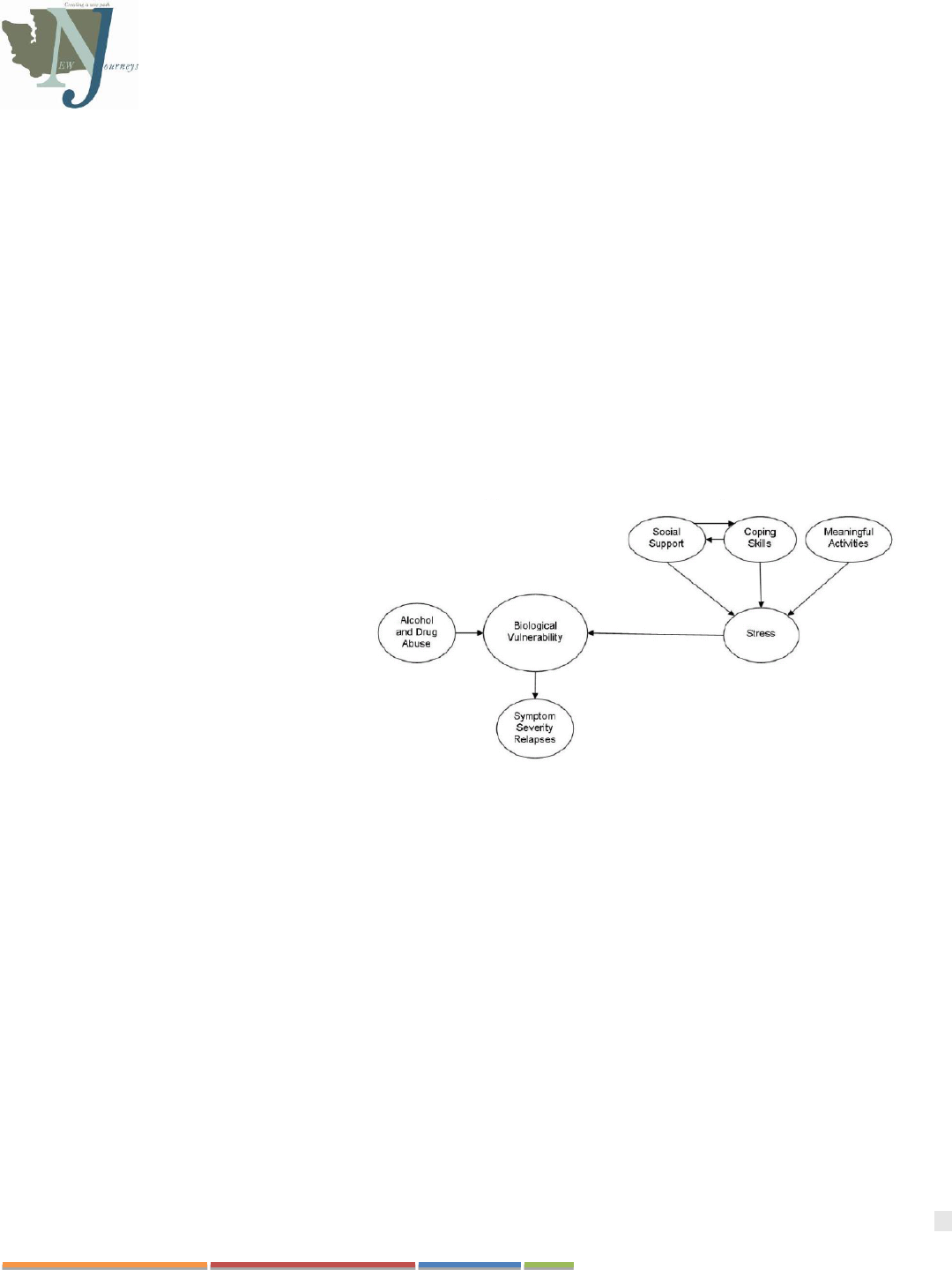
The Stress-Vulnerability Model
The Stress Vulnerability model (see Figure 6) demonstrates that schizophrenia spectrum disorders are a result of both
biological vulnerabilities and the stress an individual encounters and how they manage it. Biological vulnerabilities, or
genetic predispositions, are determined early on in life through factors of heritability and prenatal health. Ongoing
biological vulnerabilities may include alcohol and drug use and whether or not someone takes their medications as
prescribed. Stress factors, may include certain personal experiences, including adverse childhood events, lifetime trauma
exposure, and lack of adequate resources are associated with an increased risk of psychosis and schizophrenia (Varese, F.,
2012; Hunt et al, 2018). Recent research has also shown that social determinants of health such as low socioeconomic
status, urbanization, and residing in communities with low ethnic density increase risk appear to increase the risk of
schizophrenia (González-Pardo and Pérez-Álvarez, 2013; Zubin and Spring, 1997).
The indicators in the stress-vulnerability models are risk factors, not guarantees. Individuals may experience these factors
without developing psychosis. The onset and course of psychosis symptoms are impacted by these biological and
psychosocial factors and are unique to each individual.
The principles of illness management,
based on the stress-vulnerability model,
indicate that the outcomes of schizophrenia
can be improved by reducing biological
vulnerability and stress.
Stress, such as upsetting life events, can
lead to relapses and a decline in
functioning. The impacts of stress on an
individual’s vulnerability can be mitigated
through things such as positive social
support, the use of coping skills,
involvement in meaningful activities, and
access to necessary resources.
Substance abuse is another important biological factor that can impact a person’s vulnerability, leading to relapses of
psychosis and hospitalizations.
Biological vulnerability can be reduced in two ways. First, taking antipsychotic medications as prescribed can reduce
biological vulnerability by changing the way nerve tracts in the brain function. Tracts that use the neurotransmitters
dopamine and serotonin are believed to play a central role in the symptoms of schizophrenia, and the functioning of these
systems is improved by using antipsychotic medications. Second, since substance use can worsen biological vulnerability,
minimizing use and engaging in substance use treatment can also reduce this vulnerability when applicable.
Treatments that reduce stress in the environment, increase social support, or increase coping skills can also reduce
symptom severity and prevent relapses. Environmental stress in the family can be reduced by providing family education
aimed at teaching the natural supports about the nature and principles of treatment for schizophrenia, obtaining their
support for the individual’s involvement in treatment, and learning low-stress strategies for communicating and solving
problems together. Environmental stress can also be reduced by helping the individual get involved in meaningful
activities that structure the person’s time without being overly demanding. An individual’s coping skills can be bolstered
Figure 6. Stress-Vulnerability Model (Zubia and Spring, 1977)

19
Washington State New Journeys Manual – September 2023
in several ways, including providing participants with information about schizophrenia and its treatment, and teaching
them strategies for:
• Managing stress
• Monitoring symptoms
• Preventing or minimizing symptom relapses
• Coping with symptoms
• Using social skills to garner social support
Psychiatric Rehabilitation
Treatment should focus directly on helping people work towards recovery and resiliency outcomes. Three psychiatric
rehabilitation approaches are used in NAVIGATE to address different parts of recovery and resiliency; supported
employment/education targets improved role functioning and achievement of personal meaningful goals, social
rehabilitation targets social and leisure functioning, and resiliency training targets personal well-being. In addition, family
(and/or other social) support can facilitate progress toward participant goals.
• Building Hope and Resilience. New Journeys aims to support individuals in developing a sense of well-being,
including positive emotions, self-esteem, hope, and a sense of purpose. Resilience, the ability to spring back from
adverse life experiences (Neenan, 2009), is relevant when considering the life altering effect of a psychotic
episode. The IRT component of NAVIGATE emphasizes hope and resiliency. This is especially important for
people with a first episode of psychosis, who may have a sense of hopelessness and loss of control (Perry, Taylor,
& Shaw, 2007).
• Supported Education and Employment. Supported Employment is the most effective approach for improving
competitive employment outcomes in people with severe mental illness (Bond et al., 2008). A trained
employment specialist provides individual services to all participants who have a goal of gaining employment.
The goal is to find competitive work in community settings (not sheltered or transitional work) with a rapid job
search, rather than through long vocational assessments or prevocational trainings. The employment specialist
pays attention to the individual’s preferences (e.g., type of job and decision about disclosures of mental health
symptoms to employers) and provides follow-along support after the individual starts a job, rather than
discontinuing support after the individual obtains a job (Becker & Drake, 2003). The principles that have been
developed in the field of supported employment are applied by New Journeys teams to help people with FEP to
also achieve their educational goals (Killackey et al., 2008; Nuechterlein et al., 2008).
• Social Rehabilitation or Skills Training Methods. People who develop psychosis often have impaired social
functioning and may have lost friends and other social supports following a psychotic episode. In response, social
rehabilitation methods help people develop better social, leisure, and independent living functioning (Kurtz &
Mueser, 2008). To improve social skills, team members provide modeling, utilize role playing, provide feedback,
and practice of skills in sessions and in natural settings. Efforts to help social adjustment can make a big
difference in someone’s social functioning (Falloon et al., 1998; Herrmann-Doig et al., 1993; Petersen et al.,
2005).
• Family and Other Natural Supports. Family, friends, and others in a participant’s network can provide vital
social support. In addition, they can help the individual with illness management and other types of rehabilitation
and provide direct assistance in attaining goals. (Compton & Broussard, 2009; Mueser & Gingerich, 2006).
Special Issues for People Experiencing First Episode of Psychosis
New Journeys, and the NAVIGATE model, were informed by three specific challenges for many people with FEP: (1)
engagement, (2) getting back on their developmental track, and (2) processing the trauma of the onset of psychosis.

20
Washington State New Journeys Manual – September 2023
Special Issues of Engagement
Young adults utilize outpatient mental health services less than any other age group. Moreover, data suggests that 46% of
those who meet the criteria for Severe Mental Illness (SMI) do not receive treatment. Unfortunately, individuals with SMI
who do not receive treatment are at an increased risk of spending time in hospitals, jails, and crisis situations, and research
indicates youth and young adults benefit from support to navigate transitions between these situations (IOM, 2015;
CMHS, 2011; National Survey of Drug Use and Health, 2018). New Journeys provides this support during a vital time in
someone’s life through targeted community education (to facilitate identification of FEP in community settings and
through establishing and referral processes to New Journeys), enhanced engagement and outreach efforts to those referred
and enrolled in services (including seeing someone wherever they’re most comfortable including clinic, home, school, and
community settings), and meeting individuals where they are in their recovery process.
The 2022 New Journeys Annual Report demonstrates successful service utilization and improved functional outcomes for
individuals engaged with a New Journeys team, citing that individuals and their natural supports collectively attended
nearly 80% of all scheduled appointments with New Journeys teams across the state in 2022. This success is largely a
result of community-based services and the engagement and outreach provided by the team which functions to remove
barriers to accessing care and ultimately decreases dropout rates in this underserved population (Oluwoye et. al 2022).
Getting Back on Track
The onset of psychosis can knock young people off their developmental path (such as completing high school/GED, going
to college, getting their first job, developing intimate relationships, or parenting a young family). The longer psychosis
goes untreated, the more disruption in functioning the individual may experience. When an individual recently
experienced a psychotic episode, they are often acutely aware of their functional problems, which may add to feeling
demoralized and hopeless (Birchwood et al., 1998; Lewine, 2005).
For many, the first step is identifying actionable and feasible goals. When planning treatment, developmentally
appropriate goals that are based on the individual’s age, culture, family, and personal history should be identified. New
Journeys clinicians work with participants to identify and address goals that are designed to support development. This
focus helps to engage and retain people in treatment because it maximizes the relevance of the program to their lives.
Processing the Trauma of Psychosis Experiences
People who experience psychosis may experience frightening hallucinations and delusions. Individuals who also report
traumatic treatment experiences, such as involuntary hospitalization, physical restraints, and/or forced medication
administration Williams-Keeler et al., 1994). These traumatic experiences can lead to distressing symptoms of
posttraumatic stress disorder (PTSD), such as upsetting memories of psychotic symptoms or negative treatment
experiences, avoidance of stimuli that remind the person of the traumatic events, and increased physiological arousal
(Mueser et al., 2010). Furthermore, these events may trigger stigmatizing beliefs about mental illness that contribute to
maladaptive functioning (Corrigan, 2004; Penn et al., 2005).
Within New Journeys, there is a specific module in the IRT manual called “Processing the Psychotic Episode,” this
module can be important to help an individual process the experience of psychosis and begin feeling hopeful about the
prospect of recovery (Jackson et al., 2009). This conversation also provides the team an opportunity to address inaccurate
and stigmatizing beliefs that the individual may have. Open dialogue about psychosis can aid in enhancing an individual's
resiliency as they face the challenges before them while developing and using coping strategies. This resiliency building
process allows people to avoid developing maladaptive coping responses that may occur in the absence of targeted
treatment (e.g., withdrawal, resignation, substance use, or disengagement).
The choice, timing, and intensity of the different interventions are determined jointly by the individual, their natural
supports, and the New Journeys team. Person-centered treatment planning meetings and treatment review meetings with

21
Washington State New Journeys Manual – September 2023
the individual and family occur regularly to choose services, monitor progress toward treatment goals, and modify
treatment plans to be as responsive and helpful to the participant as possible.
Two Phases of New Journeys
In the initial phase of treatment with New Journeys, people often require intensive support and have an increased need for
outreach for engagement. This phase requires active efforts on the part of the team that is more time intensive than what is
generally available with regular outpatient services. As time goes on, and the individual's symptoms begin to stabilize, and
they take steps toward their goals, they may begin to decrease the frequency of their support from the New Journeys team
as they develop confidence moving forward with their goals. For some individuals, a greater duration of activities to assist
in engagement and stabilization may be needed while for others, this will be a brief aspect of their time with the New
Journeys team. While these typical phases are described below in greater detail, it is important to note that teams must be
responsive to the needs of an individual and service intensity may fluctuate during an individual’s time with New
Journeys.
Engagement and Stabilization Phase
During the engagement and stabilization phase of New Journeys, the treatment team works closely to engage with the
individual and their family/natural supports to assess areas of greatest need. The primary purpose of this phase is to illicit
motivation for treatment, address immediate needs, and manage distressing symptoms. New Journeys encounter data
indicates this phase lasts through the first six months of treatment, although individual experiences may vary due to
clinical status (i.e., whether the individual is experiencing acute symptoms of psychosis or whether the symptoms are
remitting). The goals of this phase are to:
• Engage the individual and natural supports in treatment, including meeting members of the New Journeys team
and having short (20 minute) meetings with each, if possible
• Initiate assessment, goal setting, and treatment planning
• Initiate and adjust medication to treat symptoms
• Address urgent basic needs, such as housing, medical problems, and legal issues
Connecting the individual and their natural supports in services as soon as possible following the psychotic episode is
critical. During this critical period, an individual’s natural supports are most likely to engage in their loved one’s
treatment and may be more open to acknowledging stress, expressing concerns, and receiving help from mental health
professionals due to a sense of urgency to stabilize a situation and better understand what is happening to their loved one.
Providing an individual’s natural supports with education during the Engagement and Stabilization phase can immediately
start to reduce some of the guilt, blame, or depression experienced by relatives and enlist their long-term involvement in
the individual’s treatment.
Engaging an individual experiencing symptoms in New Journeys care is facilitated by both the early exploration of the
individual’s goals for treatment based on their own preferences and values and the assessment of areas of need. This work
sets the stage for treatment planning. Staff first help participants identify and set individualized treatment goals in the
Engagement and Stabilization Phase and continue this process in the Recovery/Resiliency Phase. As an individual meets
the various members of the New Journeys team and learns about their roles, they become oriented to the overall program
and hopefully gain motivation to participate in services as they begin to understand how New Journeys can help them
achieve their goals.
During the Engagement and Stabilization phase, it is important for a New Journeys participant to engage with the team's
Psychiatric Care Provider for the initiation of medications and/or management of side effects of medication. The use of
low dose antipsychotic medication is usually necessary to reduce or stop psychotic symptoms. Once psychotic symptoms
are controlled or eliminated, individuals can participate in other aspects of treatment more fully and effectively.

22
Washington State New Journeys Manual – September 2023
Pharmacological treatment often helps engage participants by reducing distressing symptoms as staff try to understand
and work with them to address their most prominent concerns.
For many participants and their families, the ability of the New Journeys team to resolve urgent individual and/or family
needs is a prerequisite for successful engagement in the model. Case Management addresses these urgent needs such as
housing, health, and legal issues. As the team addresses basic needs and develops a therapeutic relationship with the
individual, stress on both the individual and their families/natural supports can be reduced, aiding in their overall
stabilization, and thus reinforcing participation in New Journeys.
It is also key for new participants to connect to a peer specialist during the Engagement and Stabilization Phase.
Participants often appreciate the opportunity to talk to someone who has experienced their own mental health challenges,
which can help them to feel less isolated and more hopeful about their future.
The Recovery/Resiliency Phase
Once stabilization efforts have been made, the Recovery/Resiliency Phase can begin. During this phase, individuals are
often more able/ready to engage fully in the various interventions within New Journeys. While an individual likely has
begun engaging with the various interventions prior to six months of engagement, they are often better able to utilize these
supports as their treatment progresses.
The length of this phase varies depending on each individual’s needs and progress toward their personal goals. Most
individuals will remain active in New Journeys treatment for two years. Collaborative treatment planning meetings,
including the individual and relatives or other key persons and New Journeys team members, are held at the beginning of
treatment, and occur at least every six months thereafter.
New Journeys teams typically offer all interventions to families and individuals, but there is not a requirement to
participate in everything. However, it is strongly encouraged that all participants have the opportunity to engage in all
aspects of the New Journeys model. When an intervention is offered, it is important that participants and their families are
educated about what benefit the interventions might have because it is difficult for individuals and families to make
informed decisions about participating without comprehensive information about each intervention.

23
Washington State New Journeys Manual – September 2023
CHAPTER 5: CORE COMPETENCIES OF NEW JOURNEYS TEAM MEMBERS
Core Competencies
Core competencies are the basic skills necessary for all members of the New Journeys team. They include shared
decision-making, strengths and resiliency focus, motivational enhancement skills, psychoeducational teaching skills,
cognitive-behavioral teaching skills, and collaboration with natural supports. As described above, in addition to being
trained in these core competencies by the UW Implementation Team, the Northwest MHTTC and MHTTC Network
offers an array of new, free, online training opportunities.
These competencies are described below.
Shared Decision-Making
In contrast to traditional hierarchical decision-making in which “patients” are expected to passively follow the “doctor’s
orders,” shared decision-making means that treatment decisions are made by the service recipient and clinician(s)
together, as partners, and based upon the individual’ desired goals. When family members or other natural supports are
involved in the individual’s life, they can also be involved in the decision-making process. An assumption of shared
decision-making is that the individual participant makes the decision about their treatment based on various information
they are provided about a topic to make informed decisions. This process of informed decision making often includes the
individual’s natural supports (Deegan et al., 2008). Using this perspective, each partner in the process contributes their
own specialized knowledge and experience to making decisions.
Clinicians who ignore the person’s desires or use coercion to control a participant’s treatment undermine the therapeutic
relationship (Fenton, 2003). In shared decision-making, treatment providers give evidence-based information about
treatment and the participant gives information about his or her values, goals, and preferences. The two collaborators then
discuss and negotiate a treatment plan that both believe is reasonable (Towle & Godolphin, 1999). Collaborating with
participants and respecting their ability and right as individuals to make their own treatment decisions recognizes the
choice ultimately lies with them, not the provider. This approach helps enhance the overall therapeutic relationship and
serves to empower the individual and break down internalized stigma (Corrigan, 2005).
Strengths and Resiliency Focus
Traditionally, goal setting in psychiatric treatment and rehabilitation has been focused on the reduction or elimination of
illness-related problems or “deficits,” such as symptoms, inappropriate behavior, or social withdrawal. For individuals
who have already had many setbacks in their lives, the traditional focus can worsen self-esteem. Instead, New Journeys
focuses on the strengths and resiliency factors of a person experiencing symptoms and their natural supports.
When clinicians help participants and their natural supports focus on their individual strengths and resiliency, participants
and natural supports become more aware of (and feel better about) their personal positive attributes. They become more
aware of how they have previously used these abilities to cope with life’s challenges and achieve goals, and how they can
use these attributes in the present and future. Focusing on strengths and resiliency not only makes people feel better about
themselves and their efforts, but it also helps clinicians tailor treatment to each individual and their natural supports within
their unique community.
A strengths-based approach is consistent with positive psychology, which focuses on strengths and well-being, rather than
on limitations and negative emotions. The strengths-based approach also lends to developing strategies for reaching one’s
potential and deriving meaning from one’s life, including self-acceptance, positive relationships with others, and ability to
manage day to day tasks. People experiencing FEP respond well to this focus on personal growth and developing meaning
in their life (Uzenoff et al., 2008).
24
Washington State New Journeys Manual – September 2023
Cultural Considerations
Culture has a powerful impact on the individual participant and their loved ones understanding of; a) the psychotic
experience, b) their help-seeking behaviors and attitudes, c) what matters to them in recovery, d) their preferences for
treatment, and e) their response to treatment interventions offered. Engaging individuals and their families in open
discussions about culture (e.g., their spiritual or religious beliefs, influence of their racial/ethnic backgrounds, gender
identity, experiences of marginalization or discrimination, what culturally respectful care means to them) reinforces the
process of shared decision-making and is imperative to build collaborative partnerships. Consistent with a resiliency
focus, these conversations also help identify driving cultural values, cultural/familial strengths, and skills developed
through cultural membership. It is important to remember that cultural influences (e.g., cultural messages about gender,
race, and ethnicity, religious or spiritual beliefs, beliefs about achievement, etc.) can be both constraining and enabling
toward recovery goals.
While discussing culture with participants and their natural supports, it is also important to avoid any inadvertent
assumptions about individual cultural backgrounds, to respect the constantly evolving nature of culture, and to
acknowledge cultural heterogeneity. Understanding the participants culture can help determine if any cultural adaptations
in treatment would be beneficial and can help the team identify and address cultural dilemmas that arise in their work with
service-recipients and their supports. The expression of culture in people’s lives is closely connected to other social
determinants of health, including education level, economic stability, neighborhood factors, health/access to health care
and social/community contexts (Office of Disease Prevention and Health Promotion, 2020). These determinants are
important to consider in care delivery, given the impact these could have on recovery trajectories.
New Journeys challenges old assumptions and traditional ways of thinking and introduces new ways of conceptualizing
and understanding serious mental illness. Team members are encouraged to engage in self-reflection about their own
cultural lenses and backgrounds and consider how it may influence their understandings of psychosis, treatment
recommendations, and beliefs about service-recipients. In doing so, it is important to maintain a stance of cultural
humility, or “the ability to maintain an interpersonal stance that is other-oriented or open to the other” (Hook et al., 2013,
p. 354). Additionally, cultural factors related to organizational or team culture, professional discourses about normality,
and the mental health system may be relevant to discuss, especially when they appear to be interfering with team cohesion
and/or service recipients’ recovery goals.
Motivational Enhancement Skills
Motivational Interviewing (MI) is a person-centered approach to helping individuals who are ambivalent about making
decisions or making changes in their lives. It was developed by Miller and Rollnick (Miller and Rollnick, 2013) and has
been widely adopted in settings providing treatment to people with challenges in many areas, including mental health,
substance use, physical health, involvement with the criminal justice system, school, nutrition, and weight management. It
is highly encouraged that New Journeys team members take advantage of training opportunities in motivational
interviewing. Information about training and other aspects of motivational interviewing can be found on the website.
Motivation refers to the intention and determination to follow through with an action. Problems with sustaining
motivation to follow through on desired plans and goals is one of the defining negative symptoms of schizophrenia (also
known as “avolition”). Low motivation often contributes to disengagement in treatment and problems with psychosocial
functioning. New Journeys team members can use specific motivational techniques to help participants become more
motivated.
One of the most basic approaches to enhancing the service recipient’s motivation to participate actively in treatment is the
identification and progress towards an individual’s personal meaningful goals. Clinicians may help participants to break
down long-term goals into smaller objectives and more manageable steps. Then, the clinicians can explore how learning
new information and skills (including skills about the treatment and management of one’s psychiatric disorder) can help
the participant achieve their goals.

25
Washington State New Journeys Manual – September 2023
Other examples of motivational enhancement include:
• Expressing empathy regarding the challenges the participant faces.
• Supporting self-efficacy by instilling hope that the person is capable change.
• Encouraging participants to think and dream about what they want out of their lives, and how they can achieve
their goals.
• Reframing past challenges and setbacks as opportunities to identify personal strengths and survival skills that can
be used in the future.
• Weighing the “pros” and “cons” of a health behavior (e.g., what are the advantages and disadvantages of taking
medication, getting regular exercise, or avoiding alcohol and drugs?).
• Reinforcing “change talk” when the individual is considering making a change that is consistent with treatment
recommendations or with their personal values and goals.
• “Rolling with reluctance” instead of opposing it when the individual is ambivalent about change, by affirming that
ambivalence is normal. Instead of arguing with the participant’s point of view, clinicians can explore the
individual’s ambivalence and learn more about their point of view. This helps the clinician more effectively
address the individual’s concerns about an anticipated change.
Psychoeducational Teaching Skills
Psychoeducation involves providing information about psychiatric disorders and their treatment to participants and their
natural supports. Service recipients and their supports need to understand the nature of various treatment options, and
which options are available, in order to participate in the informed, shared decision-making that is the backbone of New
Journeys.
Team members can use a variety of teaching strategies to help people understand the information taught within New
Journeys and highlight information relevant to them as individuals. Common teaching strategies include:
• Breaking down large pieces of information into smaller “chunks”
• Using and reviewing written handouts together or summarizing the content of handouts in a conversational way
• Asking questions to check understanding of information
• Inviting questions about the psychiatric disorder and its treatment
• Asking participants for their experience related to the material.
• Adopting the language of the individual and natural supports to ensure that terms and concepts are understandable
to them.
• Avoiding conflict by seeking common ground when there are disagreements between the clinician and individual
or members, or between the individual and natural supports, on topics such as diagnosis, symptoms, treatment
experiences or the explanatory model for understanding psychosis.
Cognitive-Behavioral Therapy (CBT) Teaching Skills
A broad range of CBT approaches have been developed over the past several decades for both clinical and non-clinical
populations (Bellack et al., 2004; Gingerich & Mueser, 2005; Kingdon & Turkington, 2004).
Positive verbal reinforcement is often considered the most basic and powerful of all CBT skills. Therefore, all New
Journeys team members need to be able to use positive verbal reinforcement to encourage individuals’ participation in
New Journeys, including setting personal goals, following through on home assignments, taking steps towards goals,
following treatment recommendations, and remaining actively involved in collaborative treatment planning and treatment
reviews.

26
Washington State New Journeys Manual – September 2023
New Journeys team members also need to know how to use shaping, or the reinforcement of successive approximations to
a desired goal. This means that clinicians praise even very small steps in the intended direction, such as taking steps
towards the individual’s personal goal, improvements in symptom management, or involvement in making treatment
decisions with the team.
In addition, there are many other CBT methods that are effective with FEP participants, including:
• Skills training approaches (e.g., modeling, role playing, feedback, and home practice) to teach skills for:
➢ Social situations (e.g., conversation skills, job interviewing, substance refusal, discussing medication
issues with the Prescriber)
➢ Relaxation
➢ Having fun
➢ Coping with symptoms (e.g., hallucinations)
➢ Managing urges or cravings for alcohol or drugs
➢ Developing a Relapse Prevention Plan (often called A Wellness Plan) to prevent return of symptoms of
psychosis
• Cognitive restructuring to change inaccurate or self-defeating thinking that lead to negative feelings, such as
depression, suicidal thinking, anxiety, self-stigmatizing beliefs, and distress related to psychotic symptoms.
• Self-monitoring to develop awareness of specific behaviors that may be targeted for change, such as smoking,
overeating, or use of alcohol or drugs.
• Conducting a functional or contextual analysis to aid in understanding environmental or individual factors that
contribute to or maintain behaviors of concern.
• Behavioral tailoring to incorporate new and more adaptive behaviors into the individual’s daily routine (e.g.,
taking medication) by developing natural environmental prompts for the behavior (e.g., placing the medication next
to the coffee pot so the individual is visually prompted to take it in the morning when they routinely make a pot of
coffee).
Basic knowledge of CBT teaching skills is critical to the overall success of the program, and as such, all New Journeys
team members will incorporate at least some CBT teaching into their work with the participant and their natural supports.
Collaboration with Natural Supports
“Natural supports” refers to people who have a relationship and regular contact with the individual receiving service who
can help the participant manage their psychiatric illness or make progress towards personal goals (Rapp & Goscha, 2006).
Examples of natural support include family members, friends, romantic partners, employers, and self-help group
members.
Engaging with an individual’s natural supports to take collaborative steps towards their treatment goals is important for
several reasons. First, because of their regular contact with the individual, natural supports are in an ideal position to help
individuals to take steps towards personal goals or encourage them to follow up on treatment recommendations. Second,
participants who have natural supports that are engaged in their care have fewer psychotic symptoms and better treatment
trajectories. Third, engaging with natural supports can elucidate resources that may be available to the individual that
would otherwise not have been tapped (e.g., a job lead, a useful suggestion, a potential role model). Work with natural
supports also aims to help individuals repair relationships that may have been damaged during an acute episode of
psychosis to encourage long term supportive relationships.
Finally, it’s important to note that some natural supports may inadvertently undermine the participant’s treatment
adherence (e.g., by discouraging taking medication), facilitate or encourage the use of alcohol or drugs (e.g., by
indiscriminately giving the person money that is spent on substances or using substances with the individual), or interfere

27
Washington State New Journeys Manual – September 2023
with progress towards goals (e.g., discouraging the individual from returning to school or work because of fear that stress
will provoke a relapse). Psychoeducation and skills-focused support for natural supports can help minimize these factors.
New Journeys Team Members
Each New Journeys team is staffed by an interdisciplinary team who works together to provide specialized interventions
that address the range of biological, psychological, and social needs an individual may have. Team members work in a
collaborative fashion with the individual receiving service and their natural supports. Team members must be flexible in
providing community visits and outreach. At times, the team members may be asked to work outside of typical business
hours to meet with service recipients. The team member interventions include: 1) Family Education, 2) Medication
Management, 3) Individual Resiliency Training, 4) Supported Employment and Education, 5) Peer Support Services, 6)
Case Manager and/or Nurse Case Manager (see Figure 1). The frequency of sessions or meetings is tailored to the
individual’s (and natural supports) needs, goals, and preferences.
Each team role has a team members manual (except for case management) which can be downloaded from the New
Journeys Network website.
Program Director/Family Education Provider (1.0 FTE)
The Program Director/Family Education Provider is often set up as a dual role. The ideal candidate for the Program
Director/Family Education Clinician is a licensed clinician with experience in diagnostic screening and assessment of
psychotic disorders, and expertise in working with individuals with schizophrenia-spectrum disorders and their families.
Clinicians should also have experience utilizing evidence-based practices such as multi-family groups and experience
connecting individuals and their supports with an array of tools and resources.
The Program Director monitors and oversees all team operations, leads regular team clinical meetings, and supervises the
other team clinicians. The program director is also responsible for outreach and community education (community
relations), developing a strong referral network within the agency and region, and leading the screening process for
referrals. Initially, they are the primary contact person for individuals experiencing psychosis and their families and
spearhead efforts to engage participants in the treatment model. The ideal candidate for this role has expertise in building
cross-system connections with other providers in the region.
The Family Education Clinician (sometimes also referred to as a Family Education Provider, Family Education Specialist,
FES, or simply Family Educator):
• Uses shared decision making with individuals and their families
• Provides education about psychosis and how to manage it
• Introduces and develops problem-solving skills to assist in improving communication
• Works form a strengths-based, recovery-oriented approach to psychosis
The Family Education Clinician helps an individual’s natural supports learn about psychosis and its treatment while
developing strategies for coping with stress and communicating effectively. Family education usually begins in the
engagement and stabilization phase and continues for several weeks into the recovery/resiliency phase. The Family
Education model is usually delivered over 12-14 sessions, on a weekly or every-other-week basis, with additional sessions
when needed. Some natural supports may remain engaged with Family education throughout the entire duration of their
loved one’s time with New Journeys, while others may not.
Psychiatric Care Provider (0.25 FTE)
The Psychiatric Care Provider can be a Psychiatrist or a Psychiatric Advanced Registered Nurse Practitioner (ARNP).
This team member should be experienced in working with individuals experiencing psychosis using a recovery
orientation. Medication management is guided by evidence-based practices for FEP service recipients using a shared

28
Washington State New Journeys Manual – September 2023
decision-making framework to guide individualized medication assessment and treatment. Medication treatment relies on
the use of antipsychotic medication to reduce or stop psychotic symptoms and prevent relapses, while working to
minimize side effects such as weight gain, metabolic changes, involuntary movements, and sedation.
The Psychiatric Care Provider is responsible for psychiatric diagnosis, medication management for psychiatric and
substance use disorders, acute management of suicidality and safety concerns, and physical health care needs in
coordination with the team nurse (when possible) and primary care provider. They work collaboratively with the clinical
team in treatment planning, including participating in regular team meetings and family meetings as needed.
Individual Resiliency Training (IRT) Therapist (1.0 FTE)
The IRT therapist (sometimes referred to as the IRT Clinician, IRT Specialist, or simply IRT) serves as the team’s
master’s level therapist. Individual Resiliency Training is a Cognitive Behavioral Therapy based treatment for early
psychosis. The curriculum in IRT is broken into modules and is paced on a weekly or every-other-week basis. The IRT
therapist may also participate in clinical assessment activities, as appropriate/directed by the Program Director. They work
collaboratively with the clinical team in treatment planning, including participating in regular team meetings and family
meetings.
The IRT assists with providing culturally competent, trauma-informed, strengths-based, and measurement-based care for
participants enrolled on the New Journeys team. The IRT therapist focuses on helping individuals identify and enhance
their strengths and resiliency factors, develop symptom management strategies, and teach skills to support their success in
achieving their personal goals. Examples of personal goals may include but are not limited to: engaging in meaningful
activities, employment, education, and positive relationships.
Strong candidates for the IRT position are recovery-oriented and have previous experience working with individuals with
psychosis and their supports. Clinicians should have previous experience treating young adults with:
• Psychiatric symptoms
• Substance use
• Health-risk behaviors
• Life stressors
The evidence-based therapeutic interventions included in IRT include but are not limited to:
• CBT for psychosis
• Illness Management and Recovery (IMR)
• Motivational Interviewing
• Harm Reduction
• Integrated Dual Disorder Treatment
Supported Employment and Education (SEE) Specialist (1.0 FTE)
The Supported Employment and Education (SEE) Specialist is an experienced bachelors or master’s level clinician with
experience as a supported education or supported employment specialist or as a vocational specialist. This team member
works from a recovery orientation and focuses on assisting individuals experiencing psychosis to achieve recovery goals
related to education and employment. The SEE Specialist completes most of their work outside the office. They work
collaboratively with the participant on their job search and job placement, research educational options, and provide in
vivo training in interviewing skills. In addition, the SEE Specialist provides follow-up support to individuals who have
attained a job or who are enrolled in school. It is highly desirable that the SEE Specialist have flexibility to provide
services outside of the traditional 9am-5pm work hours as needed to best support individuals in achieving their
employment and educational goals.

29
Washington State New Journeys Manual – September 2023
Supported Education and Employment services begin as soon as possible based on the participant’s preference. Even if
participants do not initially identify a desire to work or attend school, it is still important for them to have an initial
meeting with the SEE Specialist so they are aware of the supports available and can explore their interests. The SEE
Specialist works with interested individuals who choose to pursue work or education regardless of the presence of
ongoing symptoms or substance use. Services should continue to be provided throughout an individual’s time in New
Journeys to support the individual while they return to work or school.
Peer Support Specialist (0.5 FTE)
The Peer Support Specialist (sometimes referred to as the Peer Specialist or simply the Peer) has completed training in the
Washington State Certified Peer Counselor Training Program and has lived experience with mental health challenges. It is
preferred that candidates for this position have relatable experiences of psychosis to the individuals they will be serving.
Ideally, the Peer Support Specialist will be a young adult, however, anyone will be considered for the position as long as
they have an understanding of youth culture and the ability to engage with young people as a peer.
Peer Support Specialists demonstrate understanding of equity and how it intersects with service delivery. Because of the
collaborative nature of the position, peers must be able to work in changing situations with a diverse group of people,
interacting either in groups or individually. When and if appropriate, Peer Support Specialists support the individuals they
partner with through sharing their own experiences from their journey toward recovery in order to instill a sense of hope
and empowerment, while establishing and maintaining appropriate professional boundaries. If Peer Support Specialists
share their stories, they do so through a trauma-informed and culturally aware approach to support individuals with the
challenges they may be facing in their recovery and in setting and achieving goals.
Peer Support Specialists assist with engagement of individuals experiencing psychosis in services throughout treatment to
ensure that they have the information and resources they need to direct their treatment and to use an empowered voice in
the treatment planning process. The Peer Support Specialist acts as a cultural bridge between the mental health system and
the participant and their natural supports, assisting them in navigating the language and terminology of the treatment
process and the resources available. They also help in identifying needs and engaging with natural supports. Qualified
Peer Support Specialists may also assist in recovery support through facilitating or co-facilitating groups such as Illness
Management and Recovery (IMR), Wellness Recovery Action Plans (WRAP) or WRAP for work, and assisting in
Integrated Primary Care (IPC) activities, among others. Collaboration with the other clinicians on the team is key to the
peer specialist’s role.
Case Manager and/or Nurse Case Manager (0.5 FTE)
8
Case Manager
The Case Manager is a bachelors level clinician who has experience providing support to individuals experiencing mental
health challenges, including psychotic disorders and serious mental illness. As with other team member roles, this
clinician should embrace a strengths-based, recovery orientation to their work with service recipients and families. It is
vital that this team member be aware of local resources, such as housing, recreational programs, and transportation. The
Case Manager will assist with care coordination, acquiring records, treatment planning, sharing relevant resource
information, and participant scheduling. In addition, the Case Manager will track programmatic metrics to assist with
quality improvement and assurance efforts needed to maximize clinical care and participant satisfaction.
Nurse Care Manager
The Nurse Care Manager on a New Journeys team focuses on supporting healthy behaviors, wellness, and care
coordination. All New Journeys participants should have an initial nursing assessment at the beginning of treatment to
identify chronic disease risk factors and targets for self-management support (for example, regular physical activity,
8
Teams may choose to substitute a nurse care manager (~0.2 FTE) for all or part of the case manager FTE count

30
Washington State New Journeys Manual – September 2023
healthy diet, sleep hygiene, and sexual health). The Nurse also has a critical role in supporting medication management,
including providing education, monitoring for side effects, and supporting adherence to medications. In addition, the
Nurse has primary responsibility for ensuring that timely recommended metabolic monitoring is completed and tracked by
the team. The nurse typically meets with the individual experiencing psychosis weekly over the first month, every 2
weeks for the next 5 months, and then monthly during the rest of the two-year treatment, although this varies based on
individual need.
31
Washington State New Journeys Manual – September 2023
CHAPTER 6: FUNDING, SERVICE ARRAY, AND CODING
Funding and Sustainability
Startup and case building funds are provided through direct contracts with HCA/DBHR using MHBG 10% set aside
and/or Proviso funds. These funds are provided to help launch new teams while allowing them to build their caseloads
slowly over the course of 15 to 24 months. Teams are eligible to use these funds to support the startup of a New Journeys
team in their region. The use of these funds and associated invoicing processes are determined by each agency’s direct
contract with HCA/DBHR.
The New Journeys TBR 24 Month Lifetime Limit
Across the United States, most of the CSC models provide services for up to 24 months with some variation across
models (Table 3). New Journeys is based on the NAVIGATE model, which assumes a 24-month service timeline. On
average, individuals and families usually work closely (e.g., weekly) with one or more members of the team for 6 to 12
months, followed by less frequent services (e.g., bi-monthly or monthly for the next 12-18 months). Sites may use clinical
discretion to continue providing services past the 24-month mark by using regular outpatient billing processes established
by their agency as their workload allows.
Table 3. Components of CSC Programs (Wilsie & Daughtry, 2021)
State
Washington
(New Journeys)
New York
(On Track)
Oregon
(EASA)
Illinois
(First, IL)
Portland, Maine
(PIER Program)
Length
of
Service
Up to two years
(24 months)
Up to two years
(24 months)
Up to two years (24
months)
Three-five years,
pending client needs
Up to two years (24
months)
Services
• Pharmacological
Treatment
• Individual and
Group
Psychotherapy
• Case
Management
• Individual
Resiliency
Training
Therapy (IRT)
• Supported
Employment
and Education
• Peer Support
Services
• Family
Education
• Medication
Management
• Individual and
Group
Psychotherapy
• Family and
Individual
Psychoeducation
• Peer Support
• Caregiver/Family
Supports and
Services
• Educational &
Employment
Support
• Case
Management
• Structured
Behavioral
Interventions
(e.g., social and
coping skills)
• Individualized
safety planning
• Outreach and
engagement
• Assessment,
diagnosis, and
treatment planning
• Group and Individual
counseling
• Medication support
• Education and support
for individuals,
families/primary
support systems
• Crisis/relapse planning
• Navigating rights and
available benefits
• Mentoring/peer
connection
• Independent living
skills development
• Occupational therapy
• Educational and
Vocational Support
• Psychiatric care
(medications and
interventions)
• Individual resiliency
training (coping and
problem-solving
abilities)
• Supported
employment/education
• Family
psychoeducation
• Case management
(care coordination,
education on
community resources,
crisis management)
• Community
outreach and
education
• Comprehensive
assessment
• Individual and
family counseling
• Multifamily group
• Medication
Management
• Employment and
educated support
• Care management
• Care Coordination
• Psychiatric
Consultation &
Medication
• Peer
mentoring/support
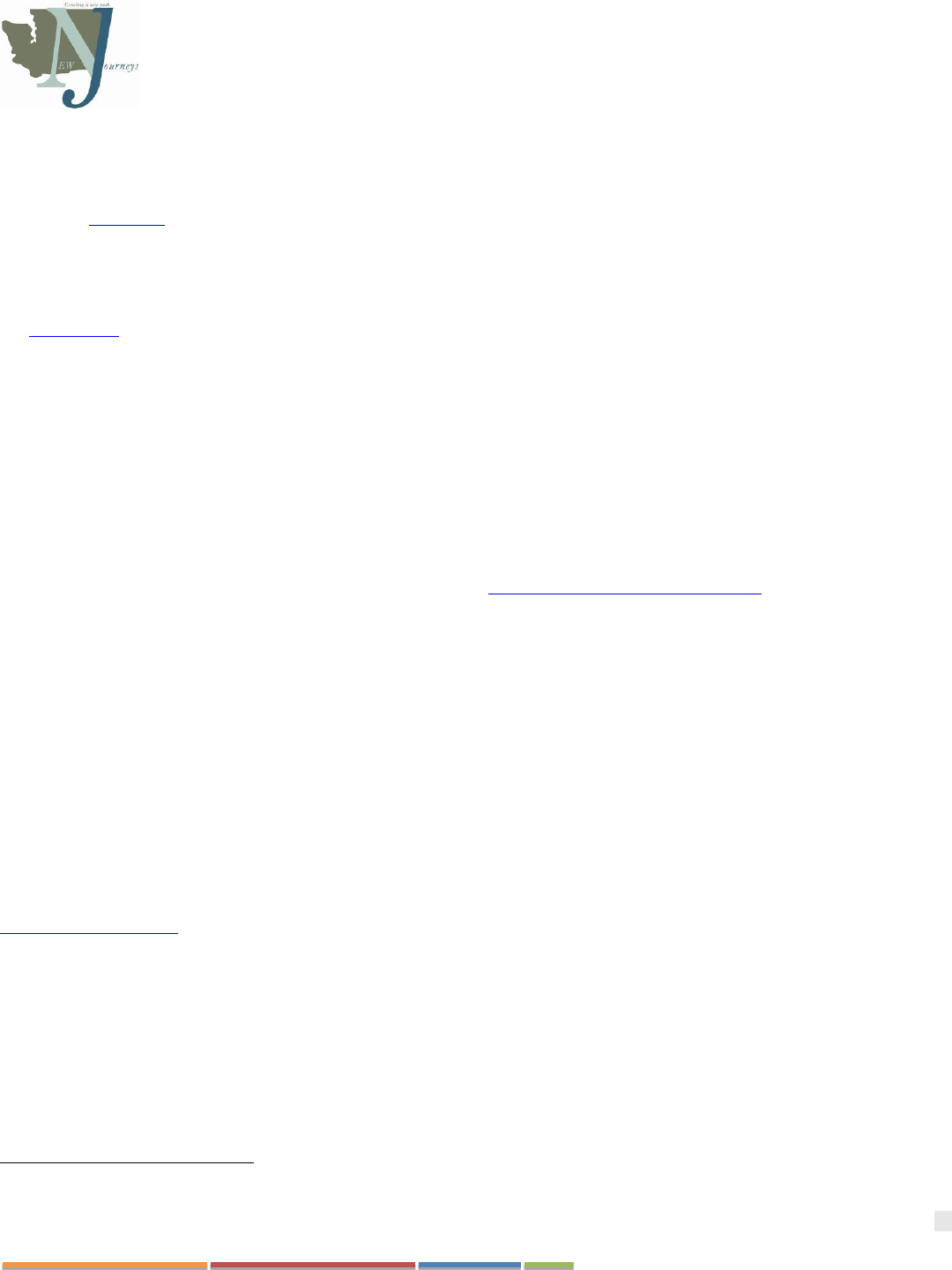
32
Washington State New Journeys Manual – September 2023
Team Based Rate
The term TBR is sometimes used interchangeably with terms like case rate, bundled payment, or service-based
enhancement. New Journeys teams typically apply to become an “Attested New Journeys Provider’ at the end of the first
year of startup and case building. The term “attested provider” refers to a team that has a) completed startup activities
outlined in Chapter 8, b) Completed the necessary training to provide New Journeys services, and c) is ready to accept
referrals. To become and attested site, an attestation form (requested from the sites HCA Contract manager) is completed
and submitted to the contract manager at HCA. This form documents that the basic New Journeys training, staffing, and
fidelity requirements have been met. Teams who are in the startup phase are NOT eligible to be added to the MCO/BH-
ASO contracts to receive the TBR (described below) and should instead use regular outpatient billing codes, outlined in
the SERI guide, to bill for direct services and use the A-19 provided by HCA/DBHR to bill for services, materials, and
other activities that are not reimbursed by insurance.
What is the Team Based Rate?
The New Journeys TBR is a two-tiered, Medicaid funded, service-based enhancement. The TBR is stratified into two tiers
to reflect the higher levels of engagement and stabilization needs during the initial 6 months of treatment and a lower level
of service provision for the remaining 18 months of the model. There is a lifetime maximum of 24 months of the TBR per
individual
9
.
▪ Tier 1: Engagement and Outreach = intake through the first 6 months of enrollment
▪ Tier 2: Recovery and Resiliency = months 7-24 of enrollment
HCA partnered with stakeholders, as directed by legislation in Second Senate Substitute Bill 5903, to develop and
implement a Team Based Rate for Medicaid. The implementation became effective July 1, 2022. In integrated care, the
New Journeys TBR is a Medicaid funded SBE that is reimbursed monthly in addition to the per member per month
(PM/PM) capitated payment. The TBR is a non-directed, team-based model with split funding which includes certain
State Plan Mental Health Outpatient services under the rehabilitative services section. The actual services delivered to
New Journeys participants will vary depending upon their individual needs and treatment plan. The TBR is determined by
an actuary process and was based upon service utilization data from the New Journeys teams in Washington. Once a New
Journeys team has an approved attestation form, the provider can access the TBR `by contracting with each of their
regions MCOs and BH-ASO’s for reimbursement through the TBR for New Journeys services.
How Does an Attested Site Bill for the Team Based Rate?
Once an attested provider has contracted with their regions MCOs and BH-ASOs, the provider will receive the New
Journeys TBR when submitting an encounter for a New Journeys eligible service. At least one service per eligible
individual during the calendar month must be entered into ProviderOne to initiate the process for payment of the TBR (see
SERI interim guidance dated 11/10/2021). The modifier “HT” must be submitted in combination with the specific,
allowed CPT/HCPCS codes on the encounter:
▪ Tier 1: Engagement and Outreach = T2022 HT
▪ Tier 2: Recovery and Resiliency = T2023 HT
Billing and reporting requirements may vary and will be defined by each provider’s MCO/BH-ASO contracts. Providers
may be expected to monitor limits to age, diagnosis, and benefit lifetime maximum to prevent accidental over billing of
the TBR.
Funding for Non-Medicaid Activities
9
The tiers to the TBR are based on averages of time and intensity of treatment. These averages assume that some individuals will need
more than 6 months of intensive engagement and outreach while others will need less intensive engagement.
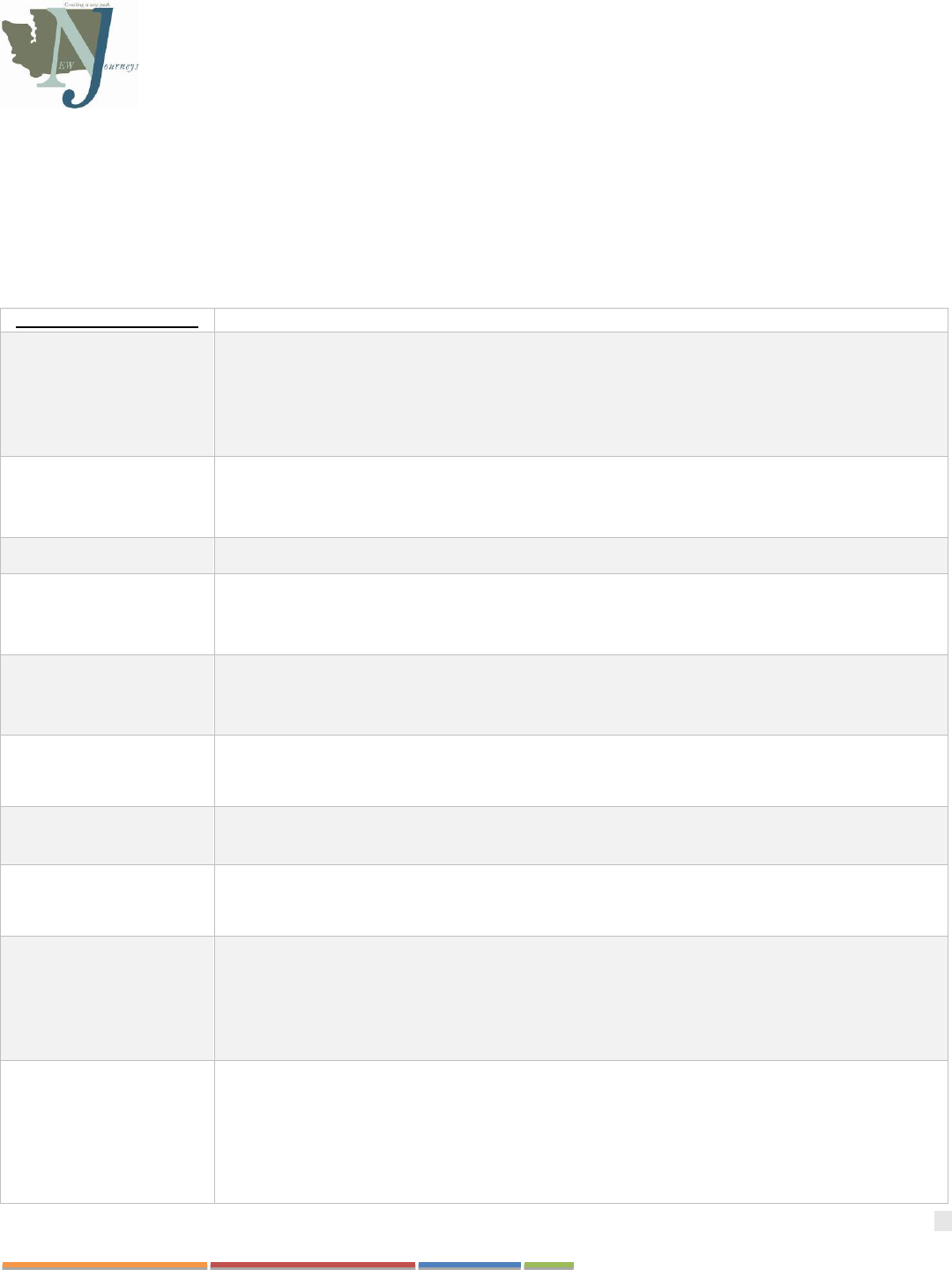
33
Washington State New Journeys Manual – September 2023
Attested New Journeys providers who are eligible for the TBR are also eligible to receive additional funds to account for
the various non-Medicaid activities they participate in as a CSC team. These state funds are made available through MCO
Wrap Contracts and should be accounted for during the contracting process with each of the regions MCOs and BH-ASO.
These non-Medicaid components of the New Journeys model are funded over and above the TBR and account for 36% of
the team's time to which is taken up in non-Medicaid activities required for New Journeys model fidelity. Examples of
non-Medicaid activities include:
Table 4. Non- Medicaid Activities Accounted for in the TBR
Non-Medicaid Activities
Examples
Concurrent delivery of
services
➢ More than one provider participating in a session based on individual request, treatment
goals, or safety
➢ Family psychoeducation w/o individual with simultaneous service w/individual (e.g., the
participant is being seen by the IRT or SEE while family psychoeducation takes place)
➢ Co-leading groups
First episode training and
consultation
➢ Training needs for New Journeys teams which are over and above provider and professional
requirements (i.e., training in the New Journeys model, attendance of monthly, role based,
consultation calls, ECHO clinics, etc.)
Fidelity review activities
➢ Peer fidelity reviews
Care coordination and
consultation
➢ Medication delivery
➢ Other case management tasks that may not meet medical necessity
➢ Collateral contacts
Time spent traveling to
community-based
appointments
➢ Staff time spent in travel w/o individual
o Searching activities
o Traveling to appointments outside of the agency’s office
Weekly multidisciplinary
team meetings
➢ Collaboration/coordination among multi-disciplinary team members
➢ Supervision needs above and beyond traditional outpatient needs
Outreach and
engagement
➢ Screening referrals both over the phone and in person prior to intake to determine eligibility
and/or engage in services
Educational and
vocational support
activities
➢ Engagement and job development with employers
➢ IEP development with the schools
Weekly and monthly
measures for WSU
evaluations (outcome
analyses)
➢ Time spent completing data entry outside of sessions
➢ Using data in real time to inform the treatment process in team meetings/treatment planning
outside of sessions
➢ Other activities needed to complete monthly metrics
➢ Monthly meetings with WSU
Other expenses
accounted for by TBR
funding:
➢ Phones
➢ Insurance
➢ Educational support items
➢ Supplies
➢ IT, EHR and computer support
➢ Capital items needed for the team

34
Washington State New Journeys Manual – September 2023
CHAPTER 7: ADMINISTRATIVE SUPPORT GUIDE
New Journeys Specific Requirements
This section will outline the infrastructure requirements a provider must have in place to be eligible for consideration as a
New Journeys provider. Each established New Journeys team must: 1) be recognized by HCA/DBHR, 2) have an
approved, current HCA/DBHR attestation, and 3) actively participate in the New Journeys Fidelity Review requirements.
For a current list of approved providers, please contact the HCA Program Manager at HCAfepinbox@hca.wa.gov.
Federal and State Requirements: The services provided under New Journeys are Medicaid services, therefore agencies are
required to meet all applicable federal standards related to the provision of mental health services covered under
Medicaid. All Behavioral Health Agencies (BHA) need a license with the Department of Health (DOH). This means that
if a group of people want to bill Medicaid using one agency NPI number, they have to be licensed with DOH. Information
on current BHAs, application process to become a BHA, and certification options can be found here: WAC 246-341-
0300.
Training and Implementation Support
The New Journeys Network and Washington State Center of Excellence in Early Psychosis (WA-CEEP) is a
collaboration between UW, WSU, and HCA that encompasses efforts to support the New Journeys Network (Network
contact list is available in Appendix G). The New Journeys Network includes an active collaboration that involves
implementation, evaluation, and quality management to support New Journeys CSC teams deliver the highest quality of
care and adhere to the purpose and goals for WA.
The WA-CEEP is fully funded by grants, contracts, and philanthropic donations to support and address four priority areas
that include:
• Providing training, consultation, implementation, and sustainability support to the Washington State New
Journeys early intervention programs to address FEP
• Educating and supporting key stakeholders in the community seeking information and resources on early
psychosis (e.g., mental health care recipients, families and natural supports, providers)
• Developing resources for the assessment and management of clinical high risk for psychosis (CHR-P)
• Advancing research on early psychosis, particularly as it relates to promoting implementation science and clinical
outcomes
Additional information about CEEP can be found at the CEEP website.
New Journeys Website and Resources
The New Journeys website and UW SPIRIT Lab website provide a comprehensive overview of the New Journeys
program as well as resources such as referral forms, team directories, training resources, and consultation and ECHO
Clinic consultation schedules. The New Journeys website also includes a secure login for New Journeys CSC team
members where additional information may be downloaded and viewed.
Among the many training materials on the New Journeys website are the NAVIGATE manuals and relevant materials
from past consultation calls.
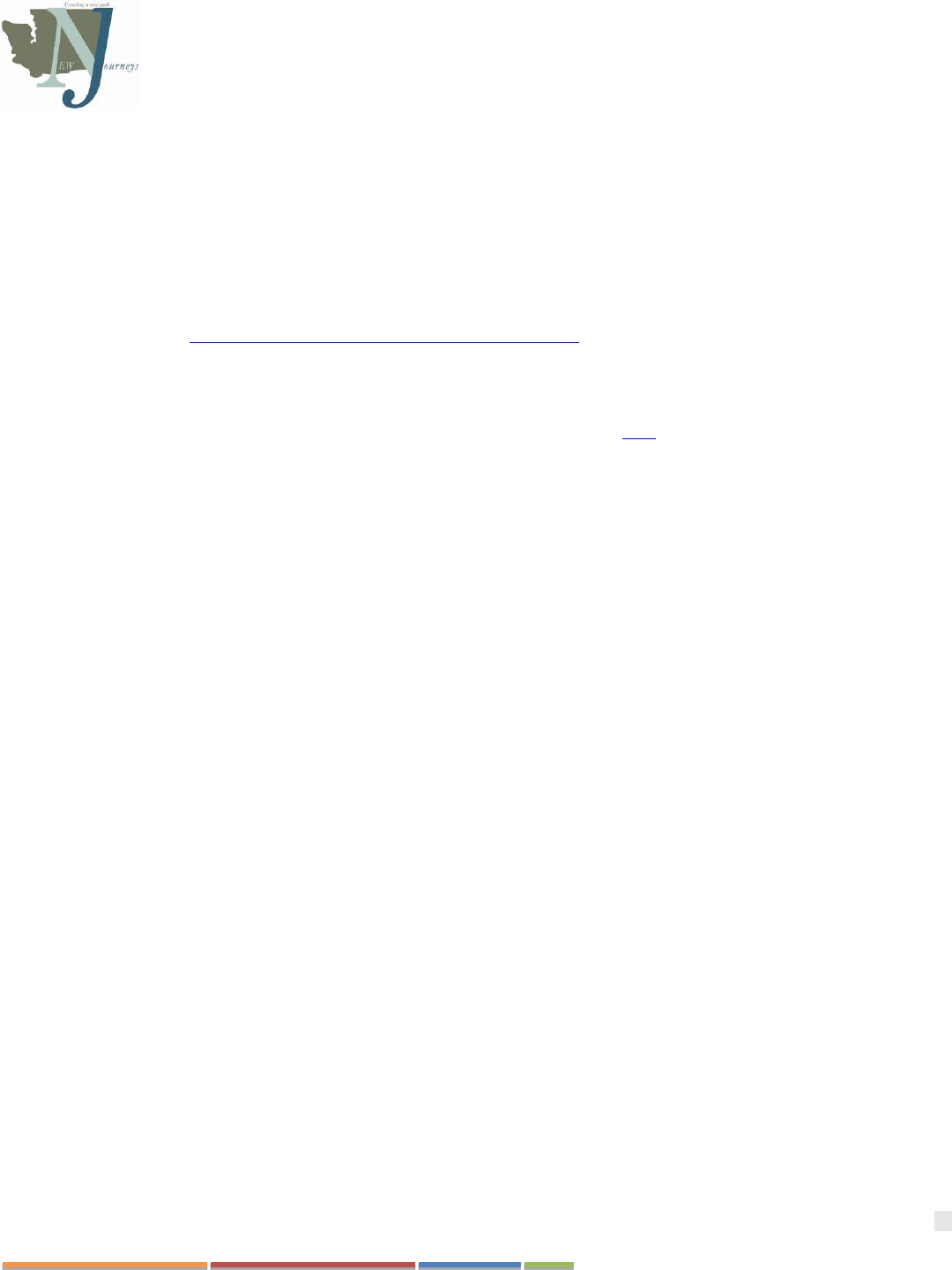
35
Washington State New Journeys Manual – September 2023
Training and Consultation
Each New Journeys team member is expected to participate in initial startup training provided by the UW Implementation
Team and WSU Evaluation Team, consisting of an orientation to CSC, New Journeys team member roles, and more in-
depth training specific to their role on the New Journeys team. In addition to start-up training, each team member is
expected to engage in ongoing monthly consultation through the following:
➢ Monthly Role-Specific Consultation calls: Program Directors, Family Education Specialists, Psychiatric Care
Providers, IRT Therapists, SEE Specialists, Nurse Care Managers, and Peer Specialists each have dedicated time
to connect with one another and receive consultation from UW specialist trainers (See current consultation call
schedule on the New Journeys website under “Consultation Calls”. Please note, there are not current consultation
calls for Case Managers).
➢ Monthly ECHO Clinics: This is a time when all of the New Journeys teams across the state meet in a virtual
format and participate in case consultation and training in topics attuned to the needs of individuals experiencing
FEP (Up to date schedule and past recordings of didactics can be found here).
➢ Training and Consultation for Screening and Differential Diagnosis: The team member(s) responsible for
screening new referrals as well as the team Psychiatric Care Providers are provided with several training resources
to assist with managing referrals and timely screening and admission:
o Structured Clinical Interview for DSM-5 Disorders (SCID-5) Training: This two-day training is
typically offered in collaboration with Ryan Melton, PhD, from the EASA Center of Excellence. The
SCID is the preferred tool for teams to use to guide initial screening for new referrals.
o Monthly Differential Diagnosis Consultation Calls: These monthly calls, facilitated by Ryan Melton,
PhD, are offered to anyone conducting screening of new referrals on the New Journeys team (see the New
Journeys website under “Consultation Calls” for the current schedule).
o Central Assessment of Psychosis Service (CAPS): CAPS extends specialized expertise in screening
and assessment of psychosis and psychosis-risk states by offering remotely delivered psychological
testing (tele-evaluation) and professional consultation (teleconsultation) to help accurately identify youth
and young adults earlier in the course of a psychotic illness. New Journeys teams that have entered into a
site-of-practice agreement with University of Washington may receive a CAPS evaluation to enhance
diagnostic accuracy for young people presenting with challenging diagnostic pictures.
➢ Training for Measurement Delivery and Data Platform: This is a time dedicated for in-depth tutorial of New
Journeys data platform, REDCAP, the set-up and use of iPad devices, and delivery of measures. These tutorials
are generally conducted virtually and allows teams to walk through the system and ask questions in the moment.
➢ Monthly Facilitation Meetings with Program Managers: WSU Evaluation team will schedule one-on-one
meetings in a virtual format with Program Directors to provide feedback on quality of data entry, address issues
with system or upcoming, gather feedback on experiences, and provide suggestions.
➢ Pat Deegan Common Ground Academy + Library: This online resource provides recovery-oriented training
and resources which compliment other materials in the New Journeys model.
➢ Quarterly Contractor Meetings: These meetings allow for regular communication between New Journeys
Contractors in the startup and case building phase with HCA. During this meeting teams will report out on their
deliverables. These meetings also allow for regular technical assistance and updates.
➢ Technical Assistance Meetings: These meetings will be scheduled with HCA to provide assistance during the
start-up and case building phases. They may be scheduled regularly, requested by the site, or requested by HCA.
In addition to these training opportunities, New Journeys team members may have other opportunities for ongoing
training. These opportunities may include specialized training on particular area of practice (e.g., Psychosis REACH
training for Family Education Specialists, CBT for Psychosis (CBTp) training for IRT Specialists, Cultural Formulation
36
Washington State New Journeys Manual – September 2023
Interview) as well as an annual New Journeys Symposium, which offers a chance for team networking and ongoing
training across the whole New Journeys Network. Another free training resource for team members to address specialized
skills and core competencies (e.g., culturally responsive care, motivational interviewing) is the Northwest Mental Health
Technology Transfer Center (MHTTC) and the MHTTC Network.
The average time that New Journeys team members spend in training and consultation specific to this evidence-based
model is 65 hours per year (see Table in Appendix B). This is in addition to an average of 48 hours of agency-based
training and other training required for licensure. This adds up to 113 training hours per clinician per year.
Fidelity Monitoring
The UW implementation team leads the annual fidelity review process utilizing the NAVIGATE-adapted version of the
First Episode Psychosis Services Fidelity Scale (FEPS-FS). Secondary co-reviewers are recruited from the New Journeys
teams, aiming for at least one trained co-reviewer per team. Fidelity reviews consist of a two-day site visit by at least two
fidelity reviewers (one from UW and one from a different New Journeys team) annually.
During the two-day site visit, reviewers will observe a team meeting, conduct interviews with New Journeys team
members, and review program documents and participant health records. After the review, the fidelity reviewers
independently rate all items on the NAVIGATE Adapted FEPS-FS, then develop consensus ratings across the 47 items.
The UW reviewer takes the lead on writing up the fidelity feedback report with input from the second reviewer, which is
then reviewed and finalized with the team. Table 5 (below) provides an estimate of team member time spent on fidelity
reviews when they are implemented in the future.
Those sites receiving startup and case building funds through direct contracts with HCA/DBHR may have extra fidelity
requirements, such as annual site visits and quarterly contractor meetings. New Journeys teams needing extra support will
be referred to the UW Implementation team for technical assistance.
Table 5. Fidelity Review
Fidelity Review Activity
Approximate Time Spent
Preparation for and participation in fidelity reviews
18 hours per year
At least one New Journeys team member trains and participates
as a secondary reviewer for the other teams’ fidelity reviews
18 hours per year (Intro training, 2 day fidelity review)
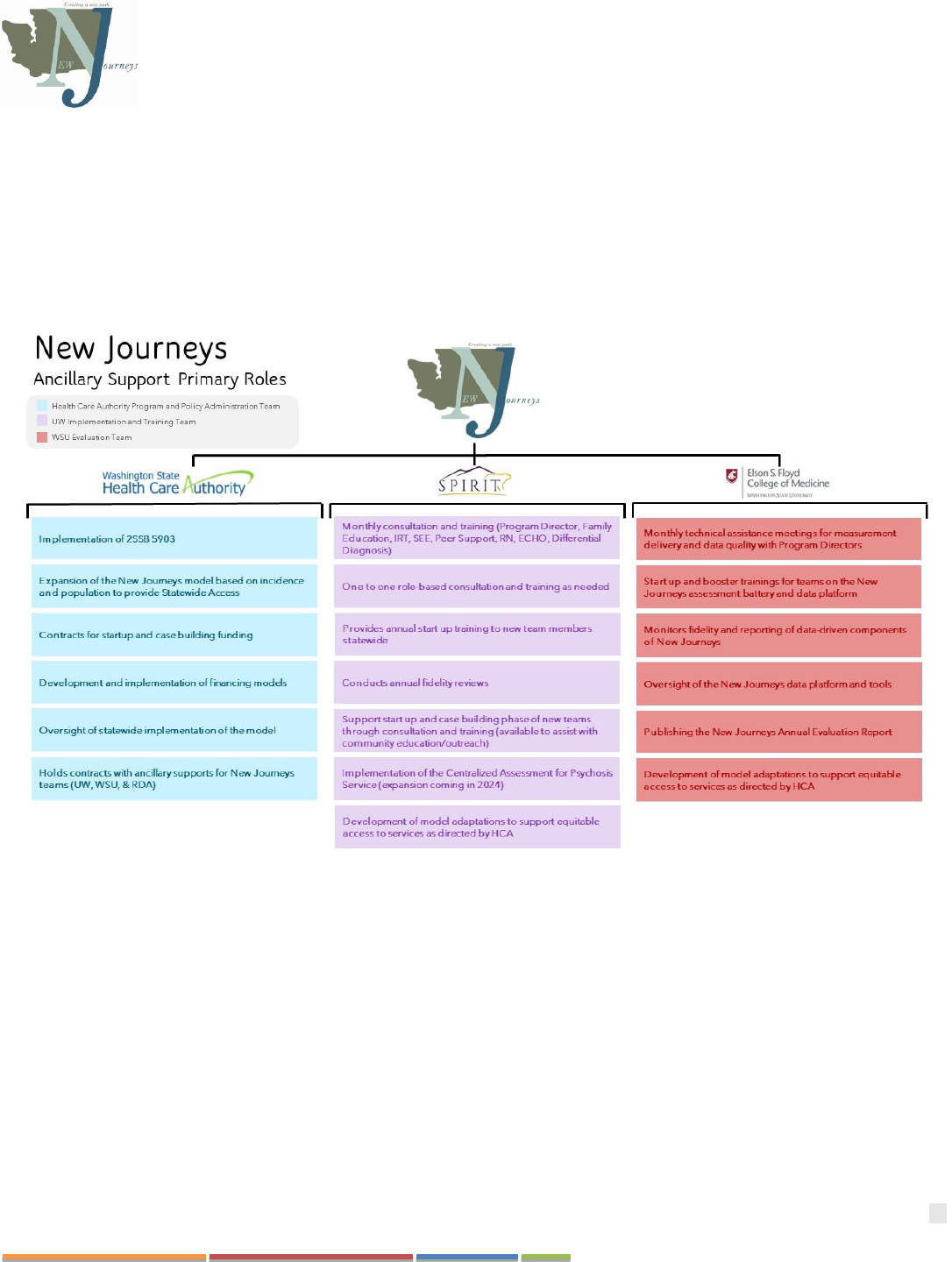
37
Washington State New Journeys Manual – September 2023
CHAPTER 8: STARTUP AND CASE BUILDING
Since New Journeys is a collaboration between HCA, UW, WSU, and various other agencies across the state, the process
of integrating into the New Journeys Network can feel complex and it can be difficult to know which entity to reach out to
for support. Figure 7 (below) was developed to assist new teams and team members in understanding the role each
ancillary support. In short, HCA’s primary role is to support funding the startup of new teams across the state, the UW
SPIRIT Lab Implementation team’s primary role is training the team members and supporting them with ongoing
consultation and education opportunities, and the WSU Measurement Delivery and Evaluation team’s primary role is the
training and implementation of measurement-based care and the evaluation of the New Journeys Network.
Figure 7. Network Ancillary Supports
Startup
New Journeys teams that are new to the network will have a period of time (referred to as the “startup phase”) before they
begin enrolling participants. The startup phase may be financially supported by a direct contract with the DBHR at the
HCA. These funds are provided to the agency or provider to cover expenses before services and encounters can be
reimbursed through other funding structures (such as insurance reimbursements), also known as “startup activities”.
Startup activities include anything that a site may need to do to establish a New Journeys team prior to providing any
direct services. This phase may last between two and six months. This varies by the region/agency in which New Journeys
is being established.
The below checklist can serve as a guide to startup activities. During startup, your primary contact for startup activities
related to HCA contracts, billing (including A-19 invoicing), and monthly reporting is your HCA Contracts Manager.
Questions related to startup, program development, community education and outreach, training, clinical consultation, etc.

38
Washington State New Journeys Manual – September 2023
can be directed to the UW Implementation Team. Any questions related to the Implementation of measurement informed
care and REDCap can be directed to each teams assigned WSU coordinator.
NEW JOURNEYS STARTUP AND CASE BUILDING CHECK LIST
This checklist provides an overview of many of the activities new sites will have to undertake during the startup and case
building phase. Activities are further identified as falling under one of the following categories:
HCA Contractual Startup Activities
☐ Determine geographic boundaries of the team being launched
☐ Contract for startup and case building financial supports
☐ Attend a “Kick-off Meeting” with HCA staff once team members are hired and the team begins taking on participants
☐ Establish monthly reporting procedures. Monthly reports document billable and non-billable deliverables within the
following categories:
1. Program Development & Implementation Activities
2. Staff Training & Professional Development
3. Community Outreach, Education, & Training
4. Participant Engagement & Outreach Services
☐ Annual submission of Attestation as an approved New Journeys site, to
be eligible to collect TBR (Medicaid Service based enhancement). Sites
are not eligible for the TBR during the first year of startup.
Program Development & Implementation Activities
☐ Become familiar with New Journeys documents and available resources
☐ Orient the leadership group and other key partners to early psychosis intervention
and how it relates to existing missions, initiatives, and priorities
☐ Develop program budget
☐ Secure adequate space for meeting referrals, conducting assessments, providing
all interventions, and attending weekly team meetings
☐ Establish access to agency vehicles or support for use of personal vehicles for
travel to community-based appointments
☐ Secure computers, tablets, and telephones for New Journeys team members
☐ Identify administrative and clerical staff to support New Journeys
☐ Once teams start case building, they should contact their HCA Contract manager
to establish a timeline for collecting the TBR, including when it would be most
appropriate for their site to establish contracts with the regions Behavioral Health
Administrative Service Organizations (BH-ASO)/ Managed Care Organizations
(MCO) for New Journeys TBR (*Eligibility begins after year one of startup)
☐ Arrange for Information Technology (IT) support
☐ Set up the agency Electronic Health Record so that individuals engaged with the New Journeys team can be identified
within the agency

39
Washington State New Journeys Manual – September 2023
☐ Arrange low barrier systems of communication to identify referrals, conduct screening and admissions, and schedule
appointments (these processes may be different from regular outpatient services intake protocols)
☐ Establish pathways to invoice all payors, including billing Medicaid and private insurance
☐ Get support for risk management, including security personnel and legal services
☐ Connect and develop protocols with the local crisis response system such as Designated Crisis Responders (DCRs)
and Evaluation & Treatment (E&T) centers for the purpose of after-hours alerts and referrals from the community
☐ Develop partnerships with adjacent New Journeys teams based on service location
☐ Establish an intake process that aligns with New Journeys specialized outreach and screening expectations and with
the agencies existing protocol (example in Appendix C)
☐ Establish processes for managing referrals outside of Medicaid
☐ Establish internal protocols for accepting internal and external referrals into the New Journey’s program within the
agency
☐ Plan for securely storing Protected Health Information (PHI) and sensitive data
Team Development
☐ Orient to the New Journeys Network and a contact person with HCA, UW, and WSU
☐ Recruit and hire New Journeys Team members (sample HR approved job descriptions in Appendix A)
☐ Develop team norms
☐ Establish team schedule for training and supervision (block these things out on the clinicians’ calendars)
☐ Engage in team building activities
Staff Training & Professional Development
☐ Ensure that all team members have relevant copies of manuals and handouts
☐ Coordinate within the New Journeys Network to complete onboarding with UW and WSU, including attendance of
clinical trainings for team member roles, Differential Diagnosis, etc. (recordings of previous trainings available here)
☐ Complete orientation with WSU to initiate data collection protocols using the New Journeys measurement delivery
and data platform
☐ Participate in monthly UW consultation calls (outlined in Appendix B. An up-to-date calendar of the calls can be
found here).
☐ Ensure the appropriate dates/times are blocked out on all team members calendars
☐ Complete monthly data entry and meetings with WSU
☐ Participate in Fidelity Monitoring (year 2 and beyond) and/or annual site visit with HCA dependent upon contract
requirements
☐ Establish regular time that team members can engage in cross training between roles and share tools/resources
☐ Set times for:
☐ Weekly team meeting (sometimes held more than once weekly)
☐ Supervision of staff
☐ Meeting with Agency director and/or CEO
Community Outreach & Education
☐ Develop materials and tools for marketing, early intervention education and outreach
40
Washington State New Journeys Manual – September 2023
• Ensure agency website has a New Journeys tab
• Procure brochures and flyers (some materials available on the New Journeys website and can also be requested in
print from WSU)
o If more than one agency exists in the region, collaborate with the other team(s) on establishing marketing
materials/plan
• Create a presentation for community education (example is available in Appendix D, an editable PPT version of
this document is also available from the UW Program Director Trainer)
• Centralized phone line for referrals
☐ Create and implement a community education plan
☐ Provide education/referral resources within existing agency/network
☐ Identify and coordinate with other parallel and related efforts in your region/county
☐ Establish an Advisory Committee and/or participate in existing regional committees to serve as an advisory committee
for the New Journeys team in that region (see Chapter 12 for more details)
☐ Build a SEE network by conducting outreach to employers (e.g., joining chamber of commerce, identifying groups to
join, etc.)
Participant Engagement & Outreach Services
☐ Establish plan for managing referrals, screening, and intake (including the development of referral forms as needed;
the New Journeys referral form can be found in Appendix E)
☐ Establish plan for case building, including plan to intake 2-3 individuals per month for a maximum of 30 participants
enrolled
☐ Establish timeline for soft launch and readiness to accept internal referrals
☐ Establish timeline for community launch and readiness to accept external referrals
Case Building
Once a team has worked through initial startup tasks and is ready to begin providing New Journeys services to the
community, they enter what is known as the “case building phase.” During the case building phase, teams continue to
complete/refine startup activities, such as developing procedures, building a community referral base, and delivering
community education. However, they are also ready to begin taking referrals.
Oftentimes, teams will start seeing participants via a soft launch. A soft launch refers to a period of time in which the only
referrals processed are from within the agency. These referrals are often identified by providers within the agency when
information about New Journeys was shared internally. These initial referrals/existing individuals who were identified as
possible candidates for New Journeys are then screened and enrolled in New Journeys if they are eligible. This soft launch
allows the new teams to begin integrating and further improving the processes they have developed for screening, referral,
and intake while also allowing team members to begin using the New Journeys model.
Shortly after, or perhaps at the same time as the soft launch, teams will begin accepting referrals from outside the agency.
Some teams will celebrate the launch of New Journeys in their community by hosting a launch event or open house. This
allows community members, stakeholders, and other resources to learn more about New Journeys and the
referral/screening process.
For New Journeys teams, it is best practice to build their caseloads incrementally over time. For a full team, it may take
between 15 and 24 months to reach full capacity, because teams should not admit more than three participants per month.
This allows teams to not only provide intensive services for new participants and refine processes for person-centered
41
Washington State New Journeys Manual – September 2023
treatment planning with the individual and their family/natural supports, but to do so while still engaging in initial
training.
This lower level of service provision also allows for completion of the Comprehensive Assessment (CA). The New
Journeys CA has three primary aims: (1) to facilitate engagement of the participant with the New Journeys team,
including developing a shared understanding of their experience and history, (2) to provide a mechanism for completing
team-based, integrated assessment and person-centered treatment planning, and (3) to incorporate measurement-based
care.

42
Washington State New Journeys Manual – September 2023
CHAPTER 9: TEAM PROCESSES
To effectively coordinate care of participants, the New Journeys team members are expected to participate in weekly team
meetings, supervision meetings, comprehensive assessment meetings, and person-centered treatment planning and review
meetings (these meetings are conducted with the participant and their natural supports present). The frequency, duration,
and nature of these meetings are summarized below.
Weekly Team Meetings
This meeting occurs with all members of the New Journeys team and should occur at minimum weekly, although many
teams typically meeting multiple days each week. Weekly team meetings are typically led by the Program Director and
usually last at least 60 minutes, depending on the number of participants in the program and the complexity of individual
treatment needs. The recommended agenda for a team meeting is as follows:
• Team members share examples of positive things that have happened with participants and families over the past
week.
• Program director shares a brief update on recruitment and enrollment.
• Team reviews each enrolled individual, starting with a quick reminder of the individual’s strengths and goal(s),
followed by a brief report from each team member. During this review, identify challenges and make plans to
address them, including who plans to do what and when. Each team member gives input on their work with the
individual and/or an individual’s natural supports, such as:
o Psychiatric Care Provider: medication issues, side effects, and symptom management
o Family Education Clinician: engagement and involvement of an individual’s natural supports, what
module they are covering in family education, any issues or concerns
o IRT Specialist: individual engagement and involvement, what module they are covering in IRT, any
issues or concerns, and opportunities for team members to reinforce or elicit adaptive behaviors
o SEE Specialist: individual engagement and involvement, what stage they are at with SEE (e.g., career
Inventory, identifying goals, job or school search, application process, employed or in school, follow-
along supports), any issues or concerns
o Peer Specialist: individual engagement and involvement, activities they are doing with the participant,
identified strengths and natural supports, and any issues or concerns
o Case Manager: individual engagement and involvement, case management activities they are doing with
the participant, any issues or concerns
• As each participant’s care is reviewed, note when their initial treatment planning meeting or their next treatment
review meeting is scheduled. If their next treatment plan is approaching, preliminary planning is done during the
team meeting to prepare. A preliminary or “penciled-in” plan is made for use during the treatment planning or
review meeting itself. Please see Appendix F for an example template for reviewing and documenting information
reviewed for each program participant in each weekly team meeting.
• At least weekly, the team should focus part of the meeting on reviewing and updating data entry and quality, as
well as cross-training between roles to help all team members learn more about how to best support each role’s
work with each participant.
Supervision Meetings
• The New Journeys Program Director meets with the IRT Specialist on a weekly basis for one hour to provide
clinical supervision for implementing the IRT intervention. If there is more than one IRT Specialist, they can

43
Washington State New Journeys Manual – September 2023
receive supervision together. Brief guidelines for supervision of IRT are provided in the Program Director’s
Manual, and more extended guidelines are in the IRT Manual.
• The New Journeys Program Director meets with the SEE Specialist on a weekly basis for one hour to supervise
the implementation of SEE and to ensure that the services are fully integrated with the other components of New
Journeys. Brief guidelines for supervision of SEE are provided in the Program Director’s Manual, and more
extended guidelines are in the SEE Manual.
• Depending on the guidelines and requirements of the agency, peer support specialists and case managers may also
receive weekly supervision with the Program Director. Brief guidelines are provided in the Program Director’s
Manual.
Comprehensive Assessment Meetings
• CA meetings should be conducted by various team members in tandem with one another as soon as the individual
and/or natural supports are engaged in services.
• Once each team member completes their respective portion of the CA, the team comes together and uses the
information gathered to complete the integrated summary sections of each section. Then, they collaboratively
complete the Putting It Together (PIT) case formulation, preferably with the individual and/or other natural
supports.
• The New Journeys Comprehensive Assessment template and a case example of the Integrated Summary and PIT
can be found on the here.
Person-Centered Treatment Planning and Review Meetings
• Within the first month of a participant’s enrollment in New Journeys, a one-hour collaborative treatment planning
meeting is held with the individual, their natural supports (if applicable), the Program Director, and any other
New Journeys team members who are or will be significantly involved in the individual’s treatment. It is
beneficial for all team members to attend; however, it is not required. Subsequent collaborative treatment review
and planning meetings are held every six months.

44
Washington State New Journeys Manual – September 2023
CHAPTER 10: MEASUREMENT-BASED CARE AND EVALUATION
Measurement-Based Care and Decision-Making
Measurement-based care (MBC) decision making is considered an evidence-based practice that typically involves the use
of standardized measures to guide treatment practice or treatment planning (Lewis et al., 2018). Studies on measurement-
based care suggest that when it is used in outpatient behavioral health settings, it improves participant outcomes (Lambert,
2002; 2003). New Journeys team members are required to collect and complete measures as part of the evaluation, but it
also serves as way assist teams in decision making and treatment planning. The New Journeys measurement battery and
data platform provides the tools (i.e., built-in measures, automatic scoring, graphical feedback) for this purpose.
New Journeys team members can use the data platform to collect and administer measures to assess individual
participants’ progress and clinical outcomes throughout treatment. Benefits to using a measurement-based care approach
include:
• Improvement to individual clinical outcomes
• The ability to observe changes over time that can be used by teams in weekly and treatment planning meetings
• Enhancement of clinician judgements with the use of objective assessments
• The ability for participants to receive feedback about their treatment progress in real time
Evaluation & Outcomes
WSU collects program specific information pertaining to outreach activities, engagement and retention of youth and
families with New Journeys, clinical outcomes of participants, and experiences from individuals and their supports. WSU
generates quarterly and yearly reports which provide both qualitative and quantitative data analysis to inform program
development and implementation.
All sites in the New Journeys network are required to utilize the New Journeys measurement-based care delivery and data
platform, which is hosted in REDCap, a system maintained through WSU. REDCap is a widely used database
management system that enables high-quality measurement collection and robust quality assurance processes. It also
provides an integrated database while simultaneously allowing remote site staff access to their participants’ data.
The New Journeys data platform incorporates several features to support the delivery of measurement-based care and
ensuring high quality meaningful data, while also maintaining confidentiality. This includes real-time data quality checks,
safety monitoring, participant calendaring system, individual case reports, and graphical feedback tools on select measures
to monitor participant progress over time. Notably, New Journey teams will only have access to their team’s data.
REDCap Server Security
WSU’s REDCap is hosted on a secure and highly available Amazon Web Service infrastructure. Some of the key aspects
of the AWS environment and infrastructure include:
➢ Deployed in an isolated, three-tiered Virtual Private Cloud on AWS
➢ Database backups are performed daily and automatically to enable operational and disaster recovery
➢ Encrypted data by default at rest and in flight (in accordance with HIPAA)
➢ Managed services to provide automated patching and maintenance of OS, middleware, and database software
➢ Assessed by WSU Information Security Services who works to protect confidentiality and integrity of data
resources and compliance with HIPAA standards.
REDCap provides the capability to remove all identifiers from our dataset prior to exporting for analysis and
reporting. There are 18 pieces of information that are considered identifiers for the purposes of HIPAA compliance.
45
Washington State New Journeys Manual – September 2023
It is important to note that not all of these identifiers are required as part of the registry and/or evaluation. The required
identifiers have been bolded:
1. Name
2. Fax number
3. Phone number
4. E-mail address
5. Account numbers
6. Social Security number
7. Medical Record number
8. Health Plan number
9. Certificate/license number
10. URL
11. IP address
12. Vehicle identifiers
13. Device ID
14. Biometric ID
15. Full face/identifying photo
16. Other unique identifying numbers,
characteristics, or codes
17. Postal address (geographic subdivisions
smaller than state)
18. Date precision beyond year
Adherence to Measurement Delivery
The WSU evaluation and measurement delivery technical assistance team will monitor measurement delivery and
completion with all New Journeys teams. WSU will meet with Program Directors monthly to discuss data quality and
completion rates and address concerns related to the REDCap platform and measurement delivery. New Journeys teams
are expected to maintain a monthly completion rate of 70% of all measures. Reports are available quarterly to each team
and are also utilized in the New Journeys Annual Evaluation Report.
Two registry forms (Information Statement and Consent Form - Client and Family/Support Person Versions) are to be
completed at the time of screening/intake; one by the individual and one by a family member/support person. These
registry forms provide teams and support persons information about key components of New Journeys and what they will
be asked to do as part of receiving services. For instance, the registry form explains how the surveys will be used to 1)
inform treatment planning by New Journeys teams; 2) evaluate the impact of each New Journeys team; and 3) evaluate
New Journeys in an aggregated way to determine the impact of the model.
In addition, participants are also asked to complete the New Journeys HIPAA release form. This form allows the New
Journeys Evaluation team to access administrative data from HCA that is used as part of the ongoing data evaluation.
Summary of New Journeys Measurement Battery
The following measures are captured in the New Journeys measurement delivery and data platform (REDCap) and can be
utilized by teams to perform measurement-based care decision-making. The New Journeys Comprehensive Assessment
provides an outline of how these measures can be used to inform care. All measures can be found in New Journeys
Measurement Battery.
Psychosis
To assess for symptoms of psychosis, the Community Assessment of Psychic Experiences – Positive Scale 15 (CAPE-
P15) is completed quarterly. The CAPE-P15 is a self-report measure that is used to assess lifetime frequency of positive
psychotic experiences. However, for New Journeys, it was modified to instead assess frequency in the last 30 days.
Fifteen questions are formatted on a Likert Scale from 0-3 with 0 being “Never” and 3 being “Nearly always”. Scores are
determined by averaging the responses across the questions the individual answered. Total scores can range from 0 – 3,
where any score greater than or equal to 1.47 indicates that the individual is currently having a clinically significant
psychotic experience. The fifteen questions are broken down into three subscales: persecutory ideation, bizarre
experiences, and perceptual abnormalities. The measure introduces a statement, for example, “In the past 30 days, have
you felt as if there is a conspiracy against you?” and the participant answers from zero to three (“never” to “nearly
always”). For any questions which were endorsed as ‘Sometimes,’ ‘Often,’ or ‘Nearly always,’ a question will populate to

46
Washington State New Journeys Manual – September 2023
have the individual rate their distress from the experience. The distress scale ranges from ‘Not distressed’ to ‘Very
distressed’. This scale is used to identify, prioritize, and address the experiences causing the individual the most distress.
The Clinician Rated Dimensions of Psychosis Symptom Severity (CRDPSS) is used to assess for symptoms of
psychosis. This measure is completed once a month by a New Journeys team member rather than by the participant. The
measure was adapted by WSU and includes 5 questions that assess the presence of: hallucinations, delusions, disorganized
speech, abnormal psychomotor behavior, and negative symptoms. Responses are on a 5-point Likert Scale (0 = “Not
present,” 4 = “Present and severe”). Each of these questions is scored independently. Scores range from 0-20. A higher
score indicates more severe psychotic symptoms.
Depression
The Patient Health Questionnaire 9 (PHQ-9) is completed monthly. The purpose is to assess for, but not diagnose,
symptoms of depression. Questions are formatted on a Likert scale from 0-3 with a maximum total score of 27. “None” is
a score less than five, “Mild” is a score from five to nine, “Moderate” is a score of ten to fourteen, “Moderately Severe” is
a score of fifteen to nineteen, and “Severe” is a score of twenty or greater. It is recommended that a score cutoff of 10 or
higher is used when detecting major depression; this would suggest further assessment by the clinical team for the
participant.
Anxiety
The Generalized Anxiety Disorder 7 Item (GAD-7) measure is completed monthly. The purpose is to assess for, but not
diagnosis, anxiety symptoms. Questions are formatted on a Likert scale from 0-3 with a maximum total score of 21.
“None” is a score less than five, “Mild” is a score of five to nine, “Moderate” is a score of ten to fifteen, and “Severe” is a
score of fifteen or greater. It is recommended that a score cutoff of 10 or higher is used when detecting an anxiety
disorder; this would suggest further assessment by the clinical team for the participant.
Functional Outcomes
This assessment identifies goals related to participant’s health, education, and employment, and is to be completed
quarterly. This measure has specific relevance to the SEE position as it tracks the participant’s goals for education and
employment, including how many days the individual attended work and school. This measure also identifies
hospitalizations, other admissions (e.g., detox facility, residential substance use treatment, crisis stabilization), and legal
involvement. This allows providers to determine sources of stress to address and support the individual more holistically.
Medical and Physical Health
To assess physical health, Medical and Physical Health Indicators are completed quarterly. This measure tracks any
changes in the individual’s weight and BMI, medication prescription and adherence, and perceived side effects from
medication which could influence care and quality of life. Individuals are also asked if they currently have a primary care
physician and the date of their most recent appointment.
Substance Use
To track an individual’s substance use across time, the Lifetime Drug Use Survey is completed at intake. The Monthly
Drug Use Survey is then completed monthly. These measures are essentially the same; however, the former asks about
lifetime use, whereas the latter asks about use in the previous month. This measure was developed using the Fagerstrom to
assess for tobacco use, and the Phenx toolkit on substance use to assess for alcohol, marijuana, and other substance use.
Participants are asked if they have ever used a specific substance or used a specific substance in the last month. If yes, it
asks how many days they used that substance. This information informs care with the treatment team. For example, if an
individual has used a substance such as cannabis and are experiencing an increase in symptoms, the IRT can integrate the
module on substance use to explore the association between substance use and the increase in symptoms. The SEE can

47
Washington State New Journeys Manual – September 2023
also apply this measure to address the effects of substance use through motivational interviewing and assessing the goals
the individual may have regarding employment, particularly if the individual’s employment requires drug testing.
Service Utilization
The Service Utilization measure is completed monthly by the providers. In this measure, providers are asked how many
sessions were scheduled for each component of the New Journeys model and how many the individual or their supports
attended. Additional positions, such as a Case Manager and Registered Nurse, are also tracked to account for all services
provided to per month. Contact, outside of scheduled appointments, with the individual and their supports are also
tracked.
OPTIONAL MEASURES
The following optional measures can be used if desired by teams to personalize their measurement-based care decision-
making.
Prodromal Questionnaire-Brief – (PQ-B)
To assess for at-risk symptoms of psychosis, the Prodromal Questionnaire-Brief (PQ-B) is completed by the clinician at
screening. The PQ-B is used to assess at-risk symptoms and distress, but not to diagnose psychosis. This measure has
twenty-one items, and if participants select yes to the corresponding question, a follow-up question will populate to have
the individual rate their distress. The distress scale ranges from ‘Strongly disagree’ to ‘Totally agree.’
Family Satisfaction
The Youth Services Survey for Families (YSS-F) is used to measure how satisfied natural supports are with the services
they are receiving. This survey tracks satisfaction across four domains: access, appropriateness, participation in treatment,
and cultural sensitivity. This measure has 26 items, all of which are rated on a 5-point Likert scale ranging from “strongly
disagree” to “strongly agree.” Two additional open-ended questions are asked regarding what the supports feel is most
helpful about services. This includes the type of services that they and their loved one have received in the last 6 months
and what could be done to improve services. This measure assists in further developing New Journeys as a model and
identifying gaps in care and services.
Discrimination Questionnaire
The Discrimination Questionnaire is completed once by the individual at intake. It assesses major discriminatory
experiences in the individual’s lifetime. This measure inquires about the participants experiences facing discrimination in
various circumstances (e.g., unfairly fired, stopped & searched by the police, discouraged from continuing education,
etc.). It also asks what they believe is the main reason for such discrimination and when it occurred. This measure assists
providers in identifying stress the individual experiences, since it can lead to worse mental and physical health including
depression and anxiety. This measure can also inform providers such as the SEE Specialist when supporting the individual
in the goals for education and employment. For example, if the individual believes they were previously discriminated
against for their sexual orientation at work, the SEE Specialist can assist the individual in finding employment at
companies who have expressed their support for the LGBTQ+ community.
COMPASS-10
The COMPASS-10 is used to assess feelings of depression, anxiety, and suicidal ideation. The Compass- 10 asks 10
yes or no questions which assess feelings of anger and suspicion, and symptoms of psychosis, including hallucinations,
disorganized speech, unusual thoughts, and negative symptoms. At the end of each question, there is a 6-point Likert
Scale (0 = “Not Present,” 6 = “Very Severe”). For some questions, additional spaces are available to allow providers to
better capture an individual’s emotional state and experiences. Providers may choose to have the individual describe how

48
Washington State New Journeys Manual – September 2023
these symptoms/emotions manifest and impact them using their own words and describe if they have talked to anyone
about these symptoms/emotions.
Process of Recovery
The Process of Recovery measure is completed quarterly and assesses positive qualities of a person’s wellbeing. It is
comprised of 15 questions each on a 5-point Likert scale ranging from “Disagree Strongly” to “Agree Strongly”. It is
advised that the measure be completed by the IRT as it can help inform strength-based recovery modules that the
individual may benefit from as well as the current level of resiliency of the participant.
Trauma Measures (CATS/LECL, PCL)
The Trauma Measure can be completed at Intake. This assesses individuals’ experiences of trauma throughout their
lifetime. There are two different measures that can be used based on the age of an individual. Individuals aged 17 and
younger should complete the Child & Adolescent Trauma Screen (CATS) while the Life Events Checklist (LECL) is
used for individuals 18 and older. When trauma is endorsed on the LECL the PTSD Checklist (PCL) should also be
completed. When trauma is endorsed on the CATS, clarifying information about how the event(s) have affected the
individual should be asked. It is advised that this measure is completed with the IRT to inform discussions about trauma
and how it may be impacting the individual’s psychosis, anxiety, or depression. This can help to guide the development of
skills to manage ongoing distress.
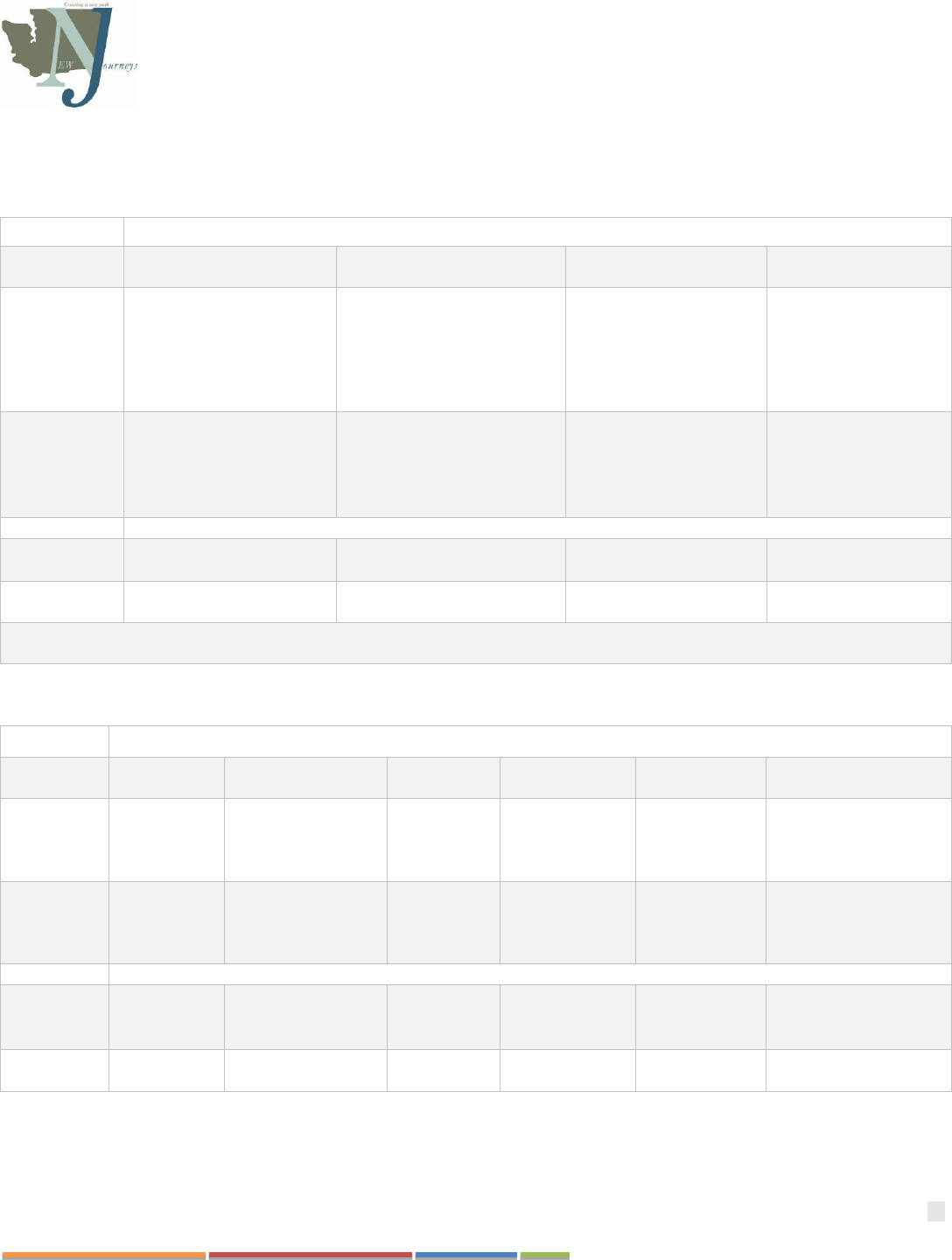
49
Washington State New Journeys Manual – September 2023
Delivery of Measures
Table 6. Measurement Delivery Across Team Members
Example 1
New Journeys Team Position
Director & Family
Education Clinician
IRT Therapist
SEE Specialist
NP/Psychiatrist
Intake Only
• Consult, Referral &
Screening
• Family Participant
Demographics
Monthly
• PHQ-9
• GAD-7
• Lifetime/Monthly Drug
Use
• CRDPSS
Service Utilization – components completed by all roles
Quarterly
Only
• CAPE-P15
• Functional Outcomes
• Medical and Physical
Health Indicators
Bi-Yearly
Only
• Demographic Follow-up
*All measures except for the demographic follow-up must be completed at baseline. Monthly measures are completed quarterly and
bi-yearly; quarterly measures are also completed bi-yearly.
Example 2
New Journeys Team Position
Director
Family Education
Clinician
IRT
Therapist
SEE Specialist
Case Manager
Nurse/NP/Psychiatrist
Intake
Only
• Consult,
Referral &
Screening
• Family
Participant
Demographics
Monthly
• PHQ-9
• GAD-7
• CRDPSS
• Lifetime/
Monthly
Drug Use
Service Utilization – components completed by all roles
Quarterly
Only
• CAPE-
P15
• Functional
Outcomes
• Medical Measure
Bi-Yearly
Only
• Demographic
Follow-up
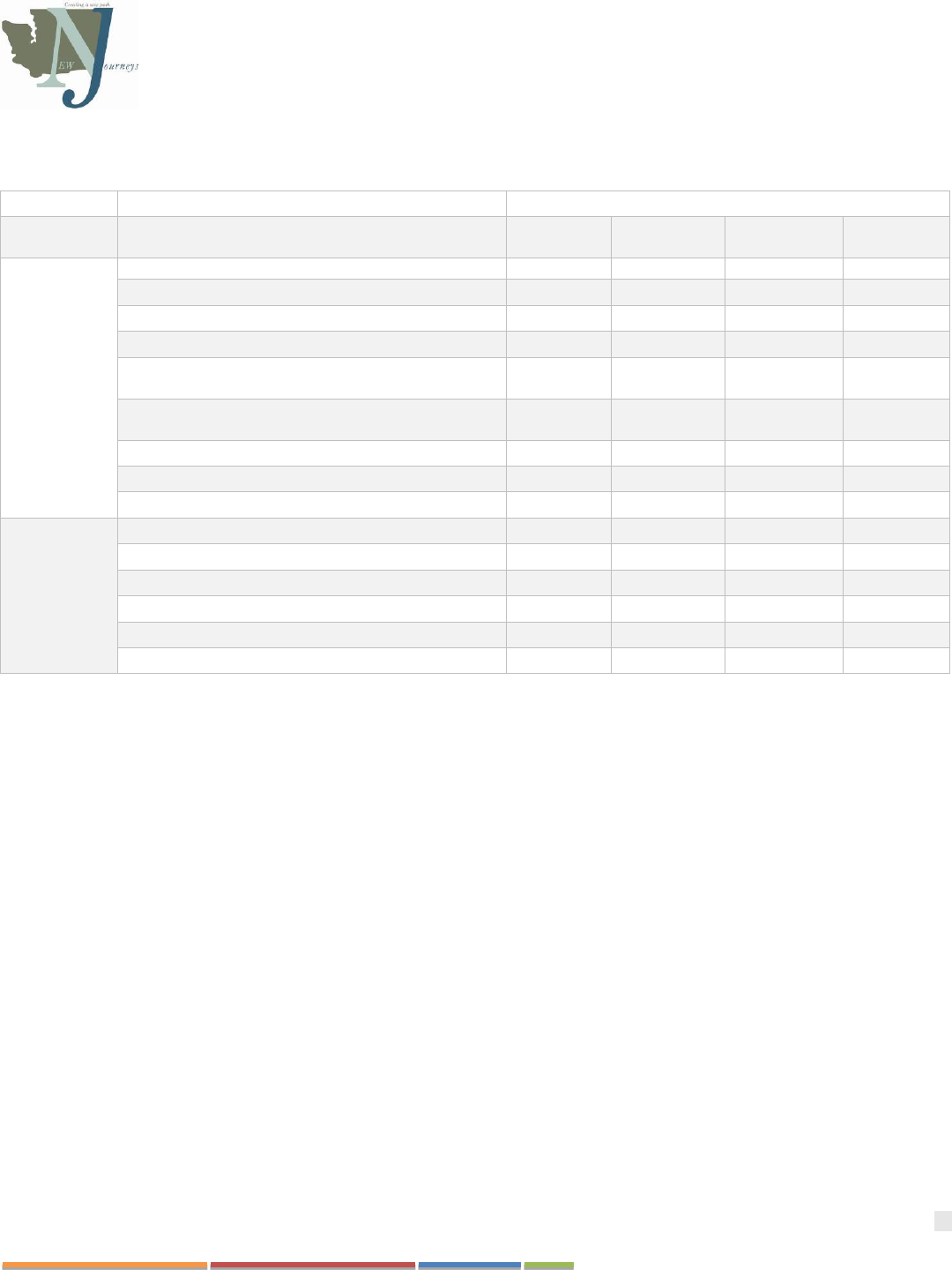
50
Washington State New Journeys Manual – September 2023
Table 6.2 Measurement Completion Frequency
Frequency
Measure
Intake
Only
Monthly
Quarterly
Bi-Yearly
Required
Patient Health Questionnaire – 9
X
Generalized Anxiety Disorder – 7
X
Functional Survey
X
Lifetime Drug Use / Monthly Drug Use
X
Clinician Rated Dimensions of Psychosis Symptom
Severity
X
Community Assessment of Psychic Experiences –
Positive 15
X
Medical Measures
X
Demographic Follow Up
X
Service Utilization
X
Optional
Prodromal Questionnaire Brief Version
X
Discrimination Scale
X
COMPASS-10
X
Trauma Measures (CATS / LECL, PCL)
X
Process of Recovery
X
Youth Services Survey for Families
X

51
Washington State New Journeys Manual – September 2023
CHAPTER 11: REDCAP ONBOARDING
New Journeys utilizes measurement-based care through the use of standardized measures that guide treatment practice and
planning. These measures are entered into and stored in an encrypted database called, REDCap. Overall, the information
that is entered into the database is used to not only inform individual treatment, but also to facilitate a better understanding
of the longitudinal clinical and functional outcomes of New Journeys teams across the state. Specifically, this information
is used in 5 different ways; 1) to generate a New Journeys Annual Report, 2) to provide additional information during the
fidelity review process, 3) to inform the need for additional training for New Journeys team members, 4) to inform
programmatic/model advancements, and 5) to advise state level decision making (including ongoing expansion,
adaptation needs, and continued funding of the model).
When new teams are in the startup phase, they connect with the WSU evaluation team to complete REDCap training. It is
advised that teams wait to complete their REDCap training until staff is hired and the team is ready to begin case building.
This gives the team the opportunity to learn how to use REDCap while utilizing the system. Many team members who
used this method noted that it facilitates improved learning and application of the database.
WSU Affiliation
Since REDCap is housed on a secure WSU server, all individuals who access REDCap must become affiliated with WSU.
All teams are assigned a WSU evaluation coordinator who will facilitate this process and ensure team members gain
access the database. Program Directors should inform their assigned coordinator when a new team member needs access
to the system in the regularly scheduled monthly meetings or by sending an email with the team members name, role on
the team, and email address. Once this information is received the WSU coordinator will send a survey to the person who
needs access, which will ask for the following information:
• Legal first name
• Legal last name
• Date of birth
• Marital status
• Gender
• Work address
• Work phone number
• Confirmation of email address
• Last 4 digits of their social security number
Those who have ever worked for, applied to, volunteered at, or were enrolled at WSU will be asked to provide their legal
first and last name and their WSU ID.
This information is used solely to establish an affiliation with WSU and will never be shared with any other party. The
information will be housed on the REDCap database until an active WSU affiliation has been established at which time all
provided demographic information from the New Journeys clinician will be removed from the REDCap database.
Once this information has been provided, a WSU New Journeys evaluation coordinator will create the affiliation and give
the New Journeys team member their WSU ID. They will be asked to create a WSU email address, password, and dual
verification (Okta account). Nobody on the WSU evaluation team will have access to any New Journeys team member’s
password or dual verification, so it is important that all affiliated personnel document their ID, email, and password in a
secure location. Should the password or dual verification not work, New Journeys team members are advised to send an
email to the Crimson Service Desk (crimsonservice[email protected]du). The Crimson Service Desk can reset passwords and
dual verifications, but will ask for confirmation of name, WSU ID, and date of birth.
52
Washington State New Journeys Manual – September 2023
Once a WSU email address is established, the New Journeys team members should tell the WSU coordinator know. The
WSU staff member will whitelist the email into a directory of people who are allowed access to the REDCap system.
The New Journeys team member then needs to log into REDCap for the first time at https://redcap.spo.aws.wsu.edu/ and
let the WSU coordinator know when they have done so. At this point the WSU coordinator will establish REDCap access
for the New Journeys team member and coordinate a training for the newly added individual.
REDCap Trainings
Once access to REDCap is established, a training will be scheduled with WSU to learn the REDCap system. One-hour
trainings are provided via Zoom on a 1:1 or group setting for teams and new hires. During this training the New Journeys
team member will learn the following:
1. How to access REDCap
2. How to review the dashboard of all current service users
3. How to add and rename new service users
4. How to input measures
5. Orientation to the Measurement Battery (including what the measures are, why they are delivered, and the
frequency of completion with service users)
6. How to track measures with the calendaring system
A second training will be scheduled no later than one week following the first so that they may have time to access
REDCap in their own time, practice entering measures or service users into the system, and then ask additional questions
they may have.
REDCap Mobile Trainings
Once a "Memorandum of understanding” form has been signed and returned to WSU, New Journeys teams are provided
with an iPad which allows the team to deliver measures while in the field, in the lobby, or in any area where they may
lack internet access. The “REDCap Mobile” app should be downloaded onto the iPad for this purpose. Teams and
individuals will participate in a one-hour training lead by the WSU coordinator on how to navigate REDCap Mobile,
including:
1. How to get access to the New Journeys project on the app
2. How to download data from the REDCap server
3. How to enter measures
4. How to upload data from the app back to the REDCap server
Refreshers on both REDCap and REDCap mobile can be provided to any New Journeys team member upon request.
Should the measurement completion rate be consistently low (≤70%), the WSU coordinator may request that the team to
be retrained, during which there will be a discussion about barriers to measurement completion and potential solutions to
these barriers.
The REDCap manuals and Measurement Battery are provided to each team prior to training. They can also be requested
or downloaded at any time from each team’s Project Dashboard under the File Repository (See Figure 8).
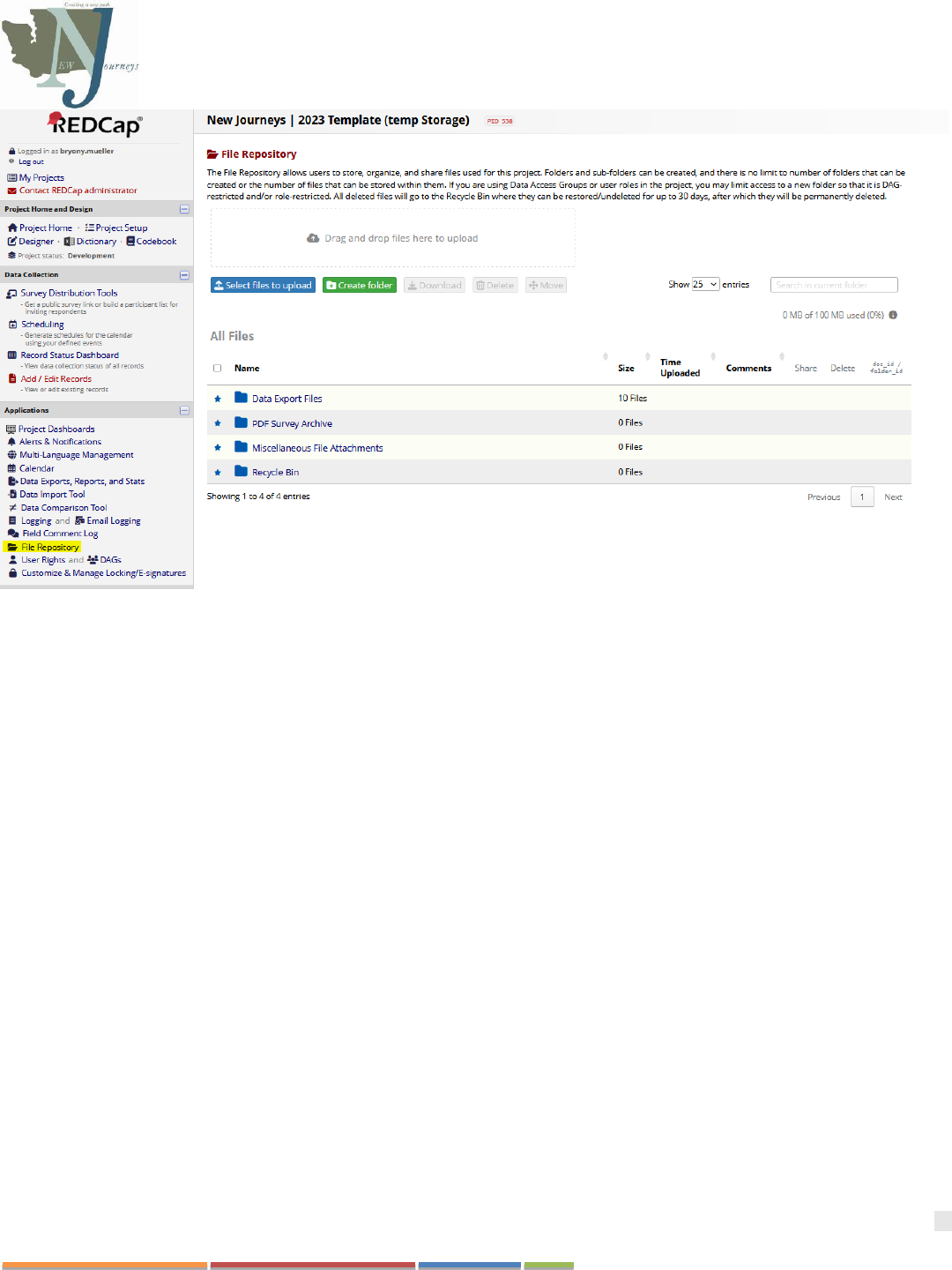
53
Washington State New Journeys Manual – September 2023
Figure 8: Image of where to access most up to date copies of the REDCap Manuals and Measurement Battery (highlight in yellow)
Any questions about trainings, measures, REDCap, or REDCap Mobile should be directed to your WSU Coordinator and
Dr. Oluwoye.
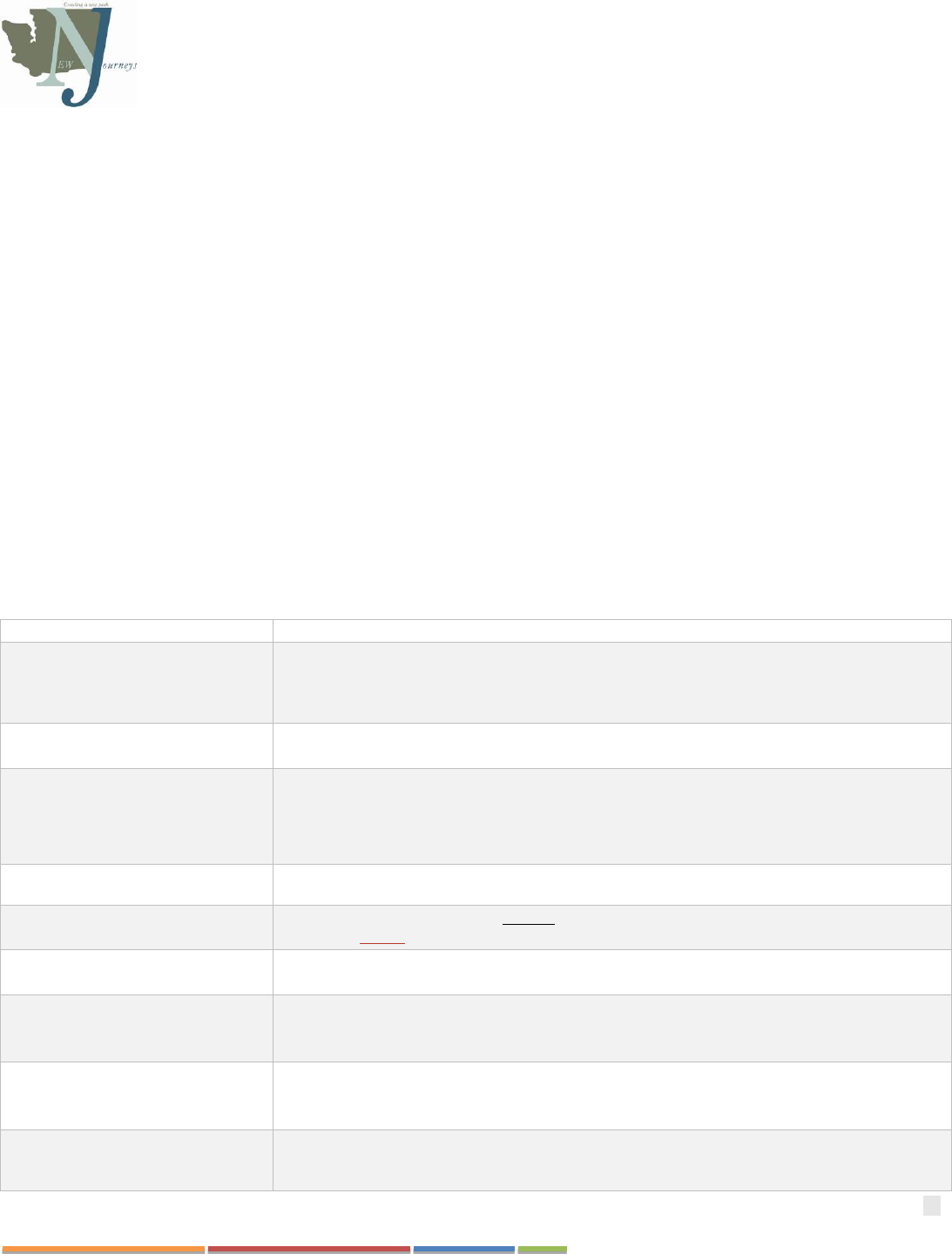
54
Washington State New Journeys Manual – September 2023
CHAPTER 12: REFERRAL, SCREENING, & ADMISSION
New Journeys teams may receive requests for consultation or other initial contacts that vary considerably, ranging from
someone experiencing a crisis, to simple questions about FEP. Due to the nature of FEP work, rapid response to referrals
and development relationships in the community are key to overall program success. Response to inquiries require prompt
response by the Program Director (usually within 72 hours).
Those referred to New Journeys will pass through up to six initial phases: 1) Request for Consultation, 2) Referral, 3)
Prescreening, 4) New Journeys Screening, 5) Agency intake, and 6) and Admission to New Journeys and/or referral to
appropriate services. Additional phases (including maintenance and discharge) will be discussed in the following chapters
of this manual.
Some agencies have found it helpful to combine stages 1-3 (Consultation, referral, and pre-screening) for ease of access.
These phases have corresponding statuses describing an individual’s pathway through New Journeys and are tracked in
the New Journeys data platform’s individual status form (See Table 4). Please refer to the New Journeys REDCap
dashboard for a full list of the most up-to-date status options.
Outside of what is included in the New Journeys measurement delivery and data platform, each agency can establish its
own protocols for how consultation is conducted and documented based on the needs of their region and requirements of
their agency. New Program Directors can reach out to other Program Directors for more information about how they have
managed these requests for consultation.
Table 7. REDCap Status Options
Status
Description
Consult Only
A consult was given to another clinician or an individual’s natural supports, during which a
member of the New Journeys team discussed whether this program was appropriate, but no
referral was made, and it was determined that the person in question was not appropriate for
services
Unable to Contact
A referral was received, but the clinician was unable to contact the person in question to
conduct a screening and determine eligibility.
Pending
A referral has been received, but the referral/screening has not taken place yet OR the
eligibility of the individual has yet to be determined as they have current circumstances which
prevent them from engaging with the program. No more than 1 month in this status.
Not Eligible
The referral and screening indicated that the individual does not meet eligibility criteria for the
program
Opted Out
The individual was determined eligible for the program; however, they chose not to
participate before receiving any services.
Active
The individual is currently enrolled in New Journeys and engaging in services by attending
sessions and participating in measurement-based care.
Provisional Admission
This status indicated that an individual has been enrolled with New Journeys with the mutual
understanding that ongoing differential diagnosis is needed to determine eligibility. No longer
than 6 months in this status.
Paused
This individual is currently in a situation where they are unable to receive New Journeys
services (e.g., currently hospitalized, in jail, etc.). Their services were paused so as not to
exceed the 24 months of allowed services they can receive from the program.
No Show
This individual has given no communication to the New Journeys team about why they are
not participating in the program. There is no known reason why they are not able to
engage. No more than 3 consecutive months in this status.
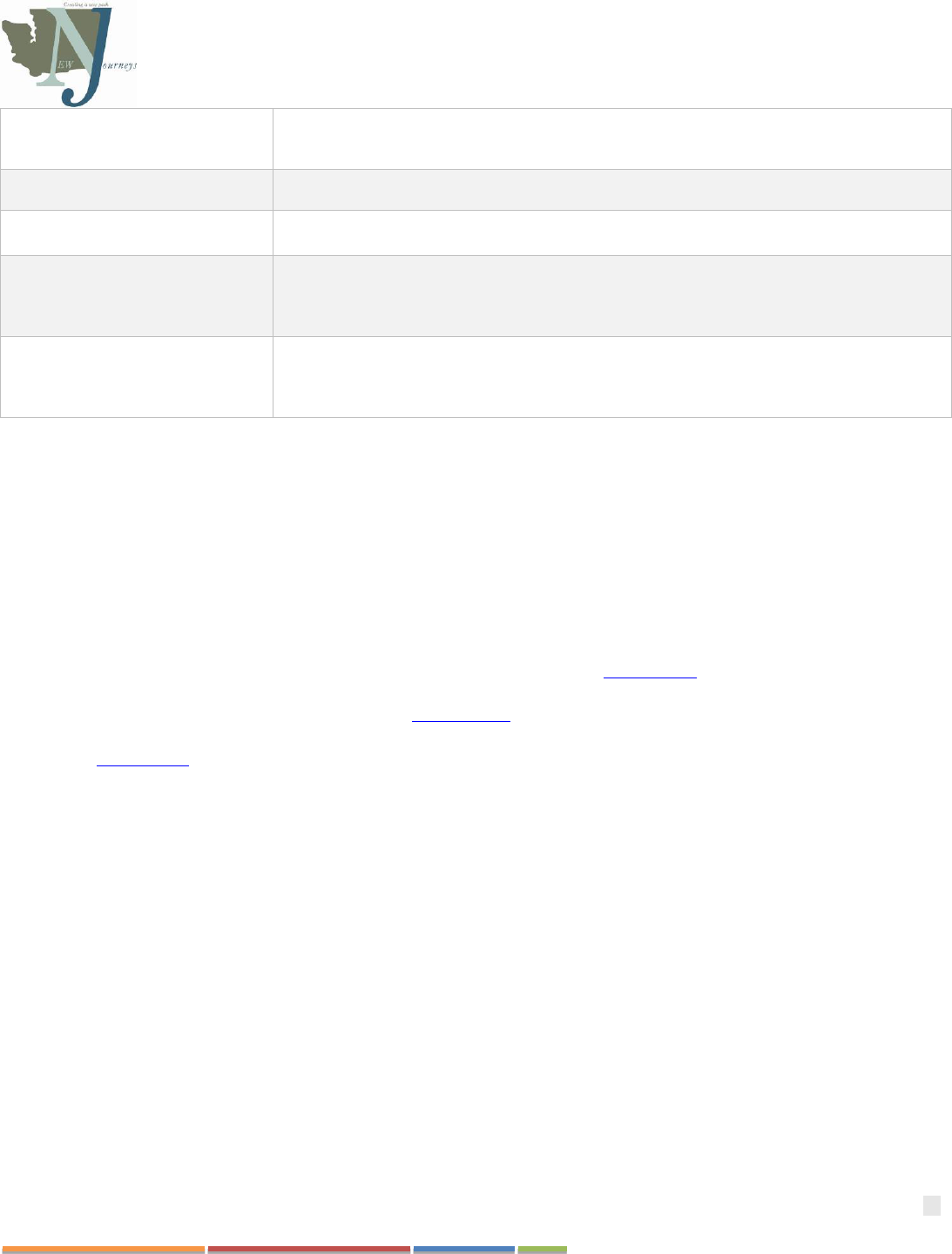
55
Washington State New Journeys Manual – September 2023
Referred to another service
While the individual was initially deemed eligible for the program, it was later determined
that this program was not the most appropriate for their needs. Clinicians coordinated with
other programs/agencies to get them the best care possible.
Referred to another New
Journeys program
The individual has relocated in Washington State and been transferred to another New
Journeys program.
Disengaged
Best attempts have been made to reengage the individual in the program, but they have not
shown up to appointments OR they requested to no longer receive services from this program.
Maintenance
This individual's next goal is graduation. The New Journeys team has lessened services and is
providing follow-up care to monitor the individual's transition process. The individual has met
the threshold for entering this phase. No more than 3 months at in this status, at which time
the individual either moves back to Active or to Graduated.
Graduated
The individual has significant improvement from their baseline appointment as indicated by
their overall wellbeing and measurement-informed care. The individual has engaged in
meaningful activities, such as school or employment, has increased socialization, and has
improved symptoms of psychosis and coping skills.
Request for Consultation
In order to ensure a successful referral system, a “no wrong door” approach is best. This means that referrals may be
received in several ways (e.g., phone, email, fax, submission of an agency’s referral form, and walk-ins). New Journeys
Program Directors may spend time in consultation with providers inside and outside of the direct agency, which may or
may not result in a formal referral to the program. These informal conversations provide opportunities for ongoing
education to providers, community members, and other referral sources in the region, and they may in turn help facilitate
appropriate referrals to the team.
Referral
During the startup phase of launching a team, a referral workflow (example in Appendix C) is created as a part of the
agency’s program development. This process will be refined as the team begins accepting referrals. Referrals can be made
in multiple ways. The New Journeys website offers a referral form which can be used to contact New Journeys teams
across the state. Most agencies also have their own referral forms (a fillable referral form that can be adapted to each
agency is in Appendix E), which should be easily accessible on the Internet. The Program Director is the central point
person who manages and oversees all referral activities and finesses the initial contact with referral sources. Referrals
should also be tracked in the New Journeys measurement delivery and data platform.
A Note on Maintaining a Referral Network
Once established, the referral network needs ongoing management and support (e.g., contact referral sources regularly,
update contact information). Even well-established teams will continue to have opportunities for community education
and refinement of referral protocols.
Decreased outreach and engagement in a region is associated with increased DUP (Weiss et al., 2022). This highlights the
importance of forming and maintaining an Advisory Committee. An Advisory Committee is comprised of cross-agency
partners who serve as liaisons to their larger agency and serve to direct FEP referrals to the New Journeys team. Members
may include representatives from various systems in the region, including but not limited to the regional BH-ASO,
MCOs, WISe Coordinator(s), allied system/agency partners (schools, youth programming, etc.), individuals with lived
experience, and/or natural supports. An Advisory Committee can enhance cross-system collaboration and improve
outcomes for youth and young adults through ongoing community education, early identification, and access to early
intervention programs. The idea is that someone experiencing FEP should be seen by the team of specialists (e.g., New
Journeys) regardless of which agency in a community the person experiencing symptoms seeks services. This may be a
different way of thinking and managing referrals than they are accustomed to. Quarterly Advisory Committee meetings

56
Washington State New Journeys Manual – September 2023
are an excellent opportunity to begin to change the narrative through educational opportunities with those external
agencies. Alternatively, some Program Directors have chosen to participate in existing community meetings/advisory
boards in their region to serve this function, rather than creating a separate advisory committee.
Pre-screening
Once a referral is received, if not already completed as a part of the consultation phase, the New Journeys Program
Director will review the referral and make contact with the referral source to complete Prescreening activities.
Prescreening activities may include contacting the referral source, making the initial contact with an individual and/or
their natural supports, and gathering records from the hospital, behavioral health agency, and/or school.
The primary purpose of the prescreening activities is to be responsive to the person seeking services and the referral
source and determine if an individual meets the most basic requirements for New Journeys, including age, duration of
psychosis, and whether the referred individual lives in the appropriate geographic area. Prescreening is typically
conducted remotely. This process can help with providing more efficient and timely feedback to referrals, as the team can
avoid conducting a full screening if the person obviously screens out due to factors such as age or geographical location.
New Journeys Screening
The Program Director determines if a formal screening is required after completing the initial prescreening of the referral
(see Table 1 for eligibility criteria).
If screening is indicated, the next step is to arrange an in-person, in-depth evaluation with the individual and their natural
supports. During this period, it may be helpful to collect additional health records and related documentation and any
other collateral information. Many Program Directors utilize the PQ-B and/or the Structured Clinical Interview for DSM-
5 (SCID-5) to assist in identifying if an individual meets New Journeys eligibility criteria. There is also a screening form
in the New Journeys data platform which should also be completed at the time of or directly after screening. This form
can serve as a checklist to indicate if an individual meets the basic New Journeys eligibility criteria.
Typically, if the diagnosis is unclear during the screening process, the Program Director should complete the SCID-5 and
use that information to guide consultation with a subject matter expert on the UW-sponsored Differential Diagnosis
Consultation Calls held monthly, or by reaching out directly to the UW training team. If further psychological,
neuropsychological, or other more extensive evaluation is indicated, the Program Director may request an evaluation
through the UW Central Assessment of Psychosis Service (CAPS; caps[email protected]).
Intake and Admission
Once it is determined that someone is eligible and interested in enrolling in services with New Journeys, the agency’s
intake protocol should be followed. Once the agency intake is complete, the participant should begin engaging in services
with the various team members. The intake marks an individual’s start date in treatment. For attested providers, the intake
will also trigger the start date of Medicaid enrollees’ TBR reimbursement schedule. At this time, the individual’s status in
New Journeys data platform should be updated to ‘Active’ and the team should complete intake measures and begin to
administer surveys as scheduled.
If the person does not meet eligibility criteria for New Journeys, or declines services, the Program Director should always
ensure a warm hand off to services more suited to the individuals’ needs. For many teams, this may mean referring
individuals to their agency’s outpatient programming, a private therapist in the community, or a more specialized program
such as WISe or Healthy Transitions for youth, or the Program of Assertive Community Treatment (PACT) for adults
with longer durations of psychosis.

57
Washington State New Journeys Manual – September 2023
Provisional Admission
It is important to note that for some individuals who present a more complex diagnostic picture and/or need more time to
further evaluate their symptom presentation, it may take months to determine eligibility. In these cases, the program
should provisionally enroll them in New Journeys, using the ‘Provisional Admission’ status in the New Journeys data
platform, while informing the individual and family/natural supports that their enrollment status may change as their
diagnosis becomes clearer over time. Provisional Admission is intended as a short-term status option (up to 6 months) to
allow a team to complete ongoing engagement and assessment of an individual’s needs. If it is determined that the
individual meets the New Journeys eligibility criteria during this period, the status in the New Journeys data platform
should be updated to ‘Active.’ During this period, if an individual is determined not to meet New Journeys criteria and is
better suited for another service, the individual should be referred to more appropriate services through the developed
referral network. The status in the New Journeys measurement delivery and data platform should be updated to ‘Referred
to Another Service.’
58
Washington State New Journeys Manual – September 2023
CHAPTER 13: ACTIVE PHASE: TIMING OF ENGAGEMENT & PROVISION OF
NEW JOURNEYS INTERVENTIONS
This section will provide an overview of the engagement process as well as some tips for beginning the various
interventions. First, it is important to note that the process of engagement with individuals and their natural supports may
vary by team and/or based on individual needs. As specific situations/questions arise, you can always reach out to a
member of the UW Implementation team (Appendix G).
Active Phase
Once an individual is enrolled in New Journeys, the Program Director and other team members will begin engaging an
individual and their natural supports in the various aspects of the model and begin providing services. This is referred to
as the ‘Active’ phase of New Journeys in the data platform. During this time, team members will engage with an
individual and their family to establish rapport, build trust, identify treatment goals, stabilize acute symptoms, and support
an individual and their natural supports in making progress toward the individual’s/family’s identified goals. These
services are described in the New Journeys manuals and in the suggested timeline of services (Table 7).
During this phase of treatment, the intensity of services is often higher, and an individual may be engaging with various
team members three to five contacts per week. This heightened service intensity is accounted for in the TBR.
Table 8. Standard Timeline of Services*
Timepoint
Family Education
Specialist
IRT Therapist
SEE Specialist
Psychiatric Care
Provider
Peer Support
Specialist
Intake
Intake and
Orientation;
Meet the team
Intake and initial
meeting
Orientation and
initial meeting
1
st
Month
Comprehensive
Assessment;
Orientation to
Family Education
Comprehensive
Assessment;
Orientation to IRT
Comprehensive
Assessment;
Orientation to SEE
services
Comprehensive
Assessment:
Orientation to
Medication
Management
Comprehensive
Assessment;
Orientation to
peer services
Collaborative
person-centered
treatment planning
meeting
Collaborative
person-centered
treatment planning
meeting
Collaborative
person-centered
treatment planning
meeting
Collaborative
treatment plan
update;
Meet weekly
Collaborative
treatment plan
update
2
nd
Month
Continue Family
Education Program
Modules; Meet
weekly or twice a
month
Begin Standard IRT
Modules; continue
to meet
approximately
weekly
Assessment and
Goal Setting-
Completion of
Career and
Education
Inventory
Meet weekly
Meet weekly
Assist participant
with work or
school goals
-School or job
search
-Help participant
with disclosure
decisions
Shift to meeting
every other week, or
continue weekly if
not yet stabilized
Meet weekly
3
rd
Month
Complete Family
Education
Program;
Treatment planning
with
recommendations
Shift to meeting
every other week, or
continue weekly if
not yet stabilized
Shift to meeting
every other
week, or
continue weekly
if not yet
stabilized
59
Washington State New Journeys Manual – September 2023
4
th
Month
Begin monthly
check-ins and
family consultation
as needed
-Participant
applications and
interviews
-Follow-along
support once
school/job has
been started
-Evaluate
participant
satisfaction and
goals;
Collaborative
treatment plan
update
Shift to meeting
every other week, or
continue weekly
when not yet
stabilized
Shift to meeting
every other
week, or
continue weekly
if not yet
stabilized
5
th
Month
Continue monthly
check-ins and
family consultation
as needed
Complete Standard
IRT Modules;
continue to meet
approximately
weekly
Shift to meeting
every other week, or
continue weekly if
not yet stabilized
Shift to meeting
every other
week, or
continue weekly
when not yet
stabilized
6
th
Month
Continue monthly
check-ins and
family consultation
as needed;
Collaborative
treatment plan
update
Begin
Individualized IRT
Modules;
Collaborative
treatment plan
update
6 month follow up
assessment and shift
to meeting monthly
if stabilized and/or
no major medication
changes;
Collaborative
treatment plan
update
Shift to meeting
every other
week, or
continue weekly
if not yet
stabilized;
Collaborative
treatment plan
update
*Case management, Peer Support, and Nurse Care Management are offered as needed throughout the participant’s time
with New Journeys. Please note that timelines can vary based on individual and family needs.
Comprehensive Assessment
The New Journeys Comprehensive Assessment is intended to support the comprehensive, ongoing collection and
integration of multiple data points in order to inform effective treatment planning. Many teams are already collecting this
information through established assessment processes within their agency. The Comprehensive Assessment can be an
additional tool to ensure that information is being shared across the team and used in a way that aids in the overall
treatment of an individual.
The New Journeys Comprehensive Assessment has three primary aims:
1. Facilitate engagement of the participant with the New Journeys team while developing a shared understanding of
their experience and history.
2. Provide a mechanism for completing team-based, integrated assessment and person-centered treatment planning.
3. Incorporate measurement-based care.
Engagement
It is crucial that team members are sensitive to an individual and their natural supports preferences regarding the extent
and intensity of services they want to receive, their needs, and their willingness and motivation to engage with the team.
Engagement can vary greatly from one individual to the next. This is expected and is why many teams consider
engagement an ongoing process throughout an individual’s time with a New Journeys team. It is important to note that
while teams remain flexible with what their engagement looks like, many agencies hold some level of expectation
regarding engagement for anyone to remain enrolled in outpatient programming within their agency. Program Directors
can educate the agency’s leadership on the unique engagement needs of those with FEP to ensure equitable access to these
services as engagement may take more time than would be expected for other outpatient programs. The Program Director
should have a clear understanding of the agency’s expectations for engagement and communicate those to the various
team members as well as those enrolling in services. Setting initial expectations for engagement can benefit the
overarching goal of early intervention, stabilization, and recovery.

60
Washington State New Journeys Manual – September 2023
It is important to inform a participant and their supports about the 24-month timeline of services early in the treatment
process. If periods of disengagement do occur, it is important that each agency follow the processes put in place within
their agency to utilize the pause feature of the TBR to preserve the 24-month lifetime benefit of the New Journeys TBR.
During the initial months of engagement, there is alignment in the curriculum taught in family education and the standard
modules of IRT. As such, coordination is needed between the Family Education Clinician and the IRT Clinician when
individuals are engaged with both.
Engagement of Individuals and Natural Supports in New Journeys
The Program Director lays a foundation for engagement while completing the referral, screening, and admission process
outlined in Chapter 12. As they are often the first person on the team to engage individuals and natural supports, the
Program Director will continue the engagement process as they facilitate introductions to the various team members and
provide an orientation to the model.
For individuals who live with (or have very engaged) natural supports, we recommend the following sequence of
engagement:
• Pre-screening/Screening- The Program Director engages with the individual, supports, and/or the referral source
to determine if the individual meets the New Journeys admission criteria and is interested in pursuing an
assessment. During this contact, the Program Director will provide a brief overview of New Journeys and the
supports offered by the team and elicit interest from the individual.
• When it is determined that the individual will enroll in New Journeys, the Program Director may revisit what is
provided in the model and review the Orientation to NAVIGATE handouts found in both the Family Education
and IRT manuals. We encourage teams to tailor this review to New Journeys and their team specifically.
• The Program Director usually tries to arrange a brief “meet and greet” with each team member. This may occur
during the screening or intake appointment as a brief introduction or can be scheduled as the first session after
intake.
• At the “meet-and-greet”, each team member can set up an initial appointment with the individual to further
explain their role and how they might be able to support the individual. These initial appointments may be brief
and may occur on the same day. This allows the participant to learn more about each team member, their role on
the team, and how the intervention can support them in making progress towards what is most important to them.
• In most cases, it is beneficial for the Family Education Clinician and the IRT Clinician to begin regular meetings
with an individual and their natural supports as soon as possible.
o If the individual agrees to their natural supports’ participation with the team, the Family Education
Clinician should meet with each of the individual’s natural supports separately to get to know them better
and assess their needs. These individual meetings can be followed by sessions where the natural supports
meet together. The individual is encouraged to attend these sessions.
AND
o The IRT Therapist should meet with the individual to begin IRT sessions, and together, they agree on a
desired frequency of initial meetings. Typically, IRT sessions occur at least weekly during the initial
phases of engagement and may decrease in frequency over time as an individual’s symptoms and needs
resolve.
• If the individual is highly symptomatic and/or still in the process of having their symptoms stabilize, the Program
Director may arrange for the individual to meet briefly with the IRT Therapist, while initiating family education
sessions with only the natural supports and postponing the first meeting with the SEE specialist and other supports
until a more appropriate time. During symptom stabilization, encouraging meetings with the Peer Specialist can

61
Washington State New Journeys Manual – September 2023
be beneficial, as the Peer can provide hope and encouragement based on their own lived experience. During this
period of stabilization, they may also find it helpful to meet with the case manager, who can assist with locating
resources to meet an individual’s most basic needs such as housing, transportation, or food as needed.
• Initial engagement can be tailored to an individual’s personal goals and preferences and based on their willingness
to engage in a particular aspect of the model. For example, an individual may choose to engage with a specific
team member they get along with most or who can offer them support in an area they are most willing to engage
with. This allows for flexibility in engagement and can help build trust with a team.
Navigating Challenges to Engagement in Family Education
Sometimes individuals will say that they do not want their natural supports to participate in their treatment. This can be
for many reasons, such as a desire to be independent of their families (e.g., “I can handle this on my own”), not wanting to
“bother” their families (“they are too busy to come to any appointments”), a history of conflict with their families (“they
don’t want to be involved with me”), or a misunderstanding about what family education sessions will entail (“family
meetings would be about people criticizing me and telling me what to do”).
When a participant expresses reluctance to have their natural supports involved, it is important to be curious about their
point of view and concerns, to talk about what family education session are and are not, and to help the individual
consider the possible advantages of their supports being involved. For example, the supports might understand better what
the individual has been going through, meeting together might help reduce conflict, or coming to family meetings might
help everyone get on the same page and support each other.
On the flip side, sometimes an individual’s natural supports will say that they do not want to be involved in family
education sessions. Like the suggestions above, it is important to be curious about their point of view and their concerns,
to dispel any misunderstandings about family education sessions, and to help them consider the possible advantages of
joining family sessions as well as their role in their loved one’s recovery process.
When participants and/or supports have not agreed to participate in family education sessions, it is important to re-visit
this topic during team meetings so the team can help problem-solve how to involve an individual’s natural supports. For
example, a participant who is reluctant to have their natural supports involved might be meeting regularly with the IRT
clinician. The IRT clinician could suggest that the family clinician join them briefly during an IRT session to talk about
the family education sessions and answer any questions the individual may have. As another example, a natural support
who is reluctant to be involved in family education might regularly accompany the individual to medication appointments.
The prescriber might broach the subject with the natural supports and even suggest that the family clinician join them for
a few minutes to answer any questions or address any concerns the support person might have.
Individuals may agree to have their supports attend family sessions but vary in terms of how much they choose to be
involved in the sessions themselves. There are three broad categories of involvement:
• The individual may be involved in all or nearly all family education sessions
• The individual may participate in only some family education sessions or may join only part of the session (e.g.,
either the first or last 20-30 minutes of the session)
• The individual may participate in no family education sessions
While it is the individuals and support person(s) choice to participate in family education sessions, the Program Director
and the rest of the team should encourage them to participate for several reasons:
1. Educating an individual’s supports about their psychiatric disorder is often more effective when the individual is
present since they can provide personal examples of their experiences and the effects of their symptoms on their
life. This may serve as a “rallying point” around which the individuals natural supports can work together.

62
Washington State New Journeys Manual – September 2023
2. Teaching the principles of treatment to the individual and natural supports together is more effective because it
involves helping the family work together to address important issues, such as taking medications as prescribed
and developing a relapse prevention plan.
3. Working with the individual and the natural supports together can alert the Family Clinician to strengths within
the family/support system that they otherwise would not have been aware of, or it can alert the Family Clinician
to the presence of problems in communication and problem-solving that would otherwise be impossible to
observe.
4. If participants and supports learn about psychosis together and become comfortable talking about it together, this
will help them continue to communicate about it in their home environment. For example, if the individual and
supports develop skills to talk about the symptom of hearing voices, if the individual begins to have auditory
hallucinations, the individual is more likely to share that information with their natural supports and the supports
are more likely to have a calm and sympathetic response. Together they may be able to reach out more effectively
to the treatment team.
Overlapping Content between Family Education and Individual Resiliency Training (IRT)
As noted above, some individuals attend family sessions along with their natural support(s) and others do not. When the
individual is actively involved in family education and attends some or all of the family sessions, IRT sessions can be
adapted to avoid overlap of educational information. As noted earlier, the educational material covered in family manual
addresses similar topics as the material in the standard modules of IRT.
Adaptations to the provision of IRT for individuals who are actively engaged in Family Education involve using IRT
sessions to briefly review any educational material covered in Family Education and to fill in any additional information
on the topics that is provided in IRT modules. Or, if the IRT sessions are covering a topic before it is covered in the
Family Education sessions, the Family sessions can briefly review the educational material covered in IRT and fill in any
additional information on the topic that is provided in the Family Education module.
63
Washington State New Journeys Manual – September 2023
CHAPTER 14: MAINTENANCE AND DISCHARGE PHASES OF TREATMENT
Maintenance Phase
As an individual’s symptoms stabilize and they begin to make progress towards their unique recovery goals, they may
require fewer services over time. As such, it may be appropriate to consider discussing moving into the “maintenance
phase.” During this phase, the team conducts a trial run of decreased supports over a period of at least three months. If this
trial goes well and the person still feels ready to graduate from New Journeys, everyone will work together to implement
the discharge plan which has been created throughout the individuals time in services.
Indicators of readiness for a maintenance phase:
• The participant indicates that they feel ready to decrease their number of appointments
• Consistent scoring (3 months or more) of 1.46 or below on the CAPE-P15 (See page 60)
• The participant made progress towards some of the goals they set for themselves
In some cases, individuals may try the maintenance phase and then require an increase in services. In this case, the team
should move their status in the New Journeys data platform back to ‘Active’ while providing increased services to meet
the individual’s needs.
Discharge
New Journeys provides intensive, time limited services to help an individual experiencing FEP to achieve a reduction in
symptoms and/or have developed skills to manage persistent symptoms, identify a path forward, and develop resiliency to
promote relapse prevention into the future. Since teams can only serve up to 30 individuals at any given time,
transitioning participants who have engaged with the treatment model is essential to ensure timely access for other
individuals experiencing FEP who need to access services.
It is important to inform a participant and their supports about the 24-month timeline of services early in the treatment
process. This introduces the narrative that experiencing psychosis does not equate to a lifetime of clinical services. As an
individual approaches 24 months in services, everyone (e.g., the New Journeys team, the individual, and their supports)
works together to decide on the next best steps to provide an individualized discharge plan. Discharge needs can vary
from person to person. Some people may transition into outpatient services offered within the agency, while others may
only need support for ongoing medication management. Many clinicians find it helpful to discuss discharge planning with
an individual throughout their course of engagement with the team. This ensures that an individual does not feel
blindsided by a transition as they approach 24 months of service. It also allows for ample opportunities to identify
supports that an individual will need after completing their time with New Journeys.
Reasons for Discharge
Eligibility Criteria is Not Met
One of the most common reasons for discharge is that the model is no longer considered to be the most appropriate
service for the participant’s needs. This may occur if it is discovered that an individual’s presentation of psychosis is not
caused by a schizophrenia spectrum disorder or may be complicated by ongoing substance use and the individual’s needs
would be better served by primary substance use services. In these scenarios, clinicians coordinate referrals with other
programs/agencies to get them the best care possible.

64
Washington State New Journeys Manual – September 2023
Disengagement or Drop-Out/Request to Discontinue Services
Other times, discharge occurs due to a team’s inability to contact a participant, known as ‘Disengagement’. In these cases,
the team has made their best attempts to contact and reengage the individual in the model. Importantly, many New
Journeys team members have communicated the need keep their cases open within the agency for longer durations of no
contact than may be typical in an agency’s outpatient programming. This need for increased flexibility is due to increased
engagement and outreach attempts, including calling the individual and natural support, visiting the individual’s home,
and sending multiple attempts to contact an individual by mail. In the data platform, the individual’s status would be “no-
show.” This status can last for up to 3 months. An individual is only discharged due to disengagement if they have not
responded to these outreach attempts, have not shown up to appointments, and/or they requested to no longer receive
services from the team.
Some individuals may ask to discontinue services or drop out. This may be because they are not ready to receive the high
level of care provided by New Journeys teams among various other reasons. The TBR accounts for this through a “pause”
feature, which acts to preserve the 24-month lifetime benefit of New Journeys and allows someone to disengage and then
return to services at a later time if needed.
Graduation
The ideal reason for discharge is graduation! When someone is eligible to graduate from New Journeys, the individual has
made significant functional improvement since enrolling with the team (indicated through engagement in meaningful
activities, improved symptoms of psychosis, and coping skills). Often these improvements are indicated by observations
of their overall wellbeing and self-report measures in the New Journeys data platform.
When someone is ready to graduate from the New Journeys team, it is important to not only make a plan for ongoing step-
down care (which may include ongoing medication management, enrollment in other services that meet an individual’s
ongoing level of care needs, engagement in self-help/peer groups, etc.) but also to consider celebrating the
accomplishment! Many teams do this through hosting small celebrations or “graduations” for the participants.
A Note on Referring to PACT/ACT Teams
When New Journeys participants are transitioning out of New Journeys services, team members often ask, “Where does
PACT (Program of Assertive Community Treatment) fit in the continuum of care for New Journeys participants?” The
goal of New Journeys is to fundamentally change the trajectory and prognosis of individuals with schizophrenia-spectrum
disorders through coordinated and systematic treatment in the earliest stages of the illness. New Journeys offers early
intervention of someone’s illness in order to prevent or limit the lifetime of disability that can be seen in more chronic
presentations of psychosis. This fundamental goal targets graduation into less intensive services. PACT, however, is a
higher level of service than New Journeys and may counteract the intention of early intervention if not referred to
appropriately.
While PACT may be a clinically appropriate transition for some participants, providers should work to ensure that they
only transition New Journeys participants into PACT if it is a clinically appropriate referral and that the team is not over-
referring New Journeys participants to PACT because it is seen as an easy transition, especially if both programs are
offered within the same agency.
As fidelity for New Journeys is developed, clinical appropriateness of individuals transitioning from New Journeys to
PACT will be assessed to ensure that when transitions do occur, they are timely, clinically appropriate, and meet the level
of care an individual continues to need after graduation from New Journeys.

65
Washington State New Journeys Manual – September 2023
REFERENCES
Adams, N., & Grieder, D. M. (2005). Treatment Planning for Person-Centered Care: The Road to Mental Health and
Addiction Recovery. Burlington, MA: Elsevier Inc.
Anthony, W. A. (1993). Recovery from mental illness: The guiding vision of the mental health service system in the
1990s. Psychosocial Rehabilitation Journal, 16, 1123.
Becker, D. R., & Drake, R. E. (2003). A Working Life for People with Severe Mental Illness. New York: Oxford
University Press.
Bellack, A. S., Mueser, K. T., Gingerich, S., & Agresta, J. (2004). Social Skills Training for Schizophrenia: A Step-by-
Step Guide (Second ed.). New York: Guilford Press.
Birchwood, M., Todd, P., & Jackson, C. (1998). Early intervention in psychosis: The critical period hypothesis. British
Journal of Psychiatry, 172 (Supplement 33), 5359.
Bond, G. R., Campbell, K., Evans, L. J., Gervey, R., Pascaris, A., Tice, S., Del Bene, D., & Revell, G. (2002). A scale
to measure quality of supported employment for persons with severe mental illness. Journal of Vocational
Rehabilitation, 17, 239250.
Bond, G. R., Drake, R. E., & Becker, D. R. (2008). An update on randomized controlled trials of evidence-based
supported employment. Psychiatric Rehabilitation Journal, 31, 280-290.
Compton, M. T., & Broussard, B. (2009). The First Episode of Psychosis: A Guide for Patients and Their Families.
New York: Oxford University Press.
Corrigan, P. W. (2004). Don't call me nuts: An international perspective on the stigma of mental illness. Acta
Psychiatrica Scandinavica, 109, 403-404.
Corrigan, P. W. (Ed.). (2005). On the Stigma of Mental Illness: Practical Strategies for Research and Social Change.
Washington, DC: American Psychological Association.
Corrigan, P. W., & Holmes, E. P. (1994). Patient identification of "Street Skills" for a psychosocial training module.
Hospital and Community Psychiatry, 45, 273-276.
de Leon, J., & Diaz, F. J. (2005). A meta-analysis of worldwide studies demonstrates an association between
schizophrenia and tobacco smoking behaviors. Schizophrenia Research, 76, 135-157.
Deegan, P. E., Rapp, C. A., Holter, M., & Riefer, M. (2008). Best practices: a program to support shared decision
making in an outpatient psychiatric medication clinic. Psychiatric Services, 59, 603-605.
Elson S. Floyd College of Medicine- Washington State University. (2022). 2022 Evaluation Report
Falloon, I. R. H., Coverdale, J. H., Laidlaw, T. M., Merry, S., Kydd, R. R., & Morosini, P. (1998). Early intervention
for schizophrenic disorders: Implementing optimal treatment strategies in routine clinical services. British Journal
of Psychiatry, 172(Suppl. 33), 33-38.
Fenton, W. S. (2003). Shared decision making: A model for the physician-patient relationship in the 21st century? Acta
Psychiatrica Scandinavica, 107, 401-402.
Gingerich, S., & Mueser, K. T. (2005). Illness management and recovery. In R. E. Drake & M. R. Merrens & D. W.
Lynde (Eds.), Evidence-Based Mental Health Practice: A Textbook (pp. 395-424). New York: Norton.
Gingerich, S. & Mueser, K.T. (2011). Illness Management and Recovery: Personalized Skills and Strategies for Those
with Mental Illness. Hazelden Publications.
González-Pardo, H., & Pérez Álvarez, M. (2013). Epigenetics and its implications for Psychology. Psicothema, 25(1),
3–12. https://doi.org/10.7334/psicothema2012.327
Green, M. F. (1996). What are the functional consequences of neurocognitive deficits in schizophrenia? American
Journal of Psychiatry, 153, 321-330.
Häfner, H., & an der Heiden, W. (2008). Course and outcome. In K. T. Mueser & D. V. Jeste (Eds.), Clinical
Handbook of Schizophrenia (pp. 100-113). New York: Guilford Press.
Häfner, H., Löffler, W., Maurer, K., Hambrecht, M., & an der Heiden, W. (1999). Depression, negative symptoms,
social stagnation and social decline in the early course of schizophrenia. Acta Psychiatrica Scandinavica, 100, 105-
118.
66
Washington State New Journeys Manual – September 2023
Häfner, H., Maurer, K., Löffler, W., an der Heiden, W., Hambrecht, M., & SchultzeLutter, F. (2003). Modeling the
early course of schizophrenia. Schizophrenia Bulletin, 29, 325-340.
Heinssen, R. K., Goldstein, A. B., & Azrin, S. T. (2014). Evidence-based treatments for first episode psychosis:
Components of coordinated specialty care. Retrieved from
https://www.nimh.nih.gov/health/topics/schizophrenia/raise/evidence-based-treatments-for-first-episode-psychosis-
components-of-coordinated-specialty-care.shtml
Herrmann-Doig, T., Maude, D., & Edwards, J. (1993). Systematic Treatment of Persistent Psychosis: A Psychological
Approach to Facilitating Recovery in Young People with First-Episode Psychosis. London: Martin Dunitz.
Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., & Utsey, S. O. (2013). Cultural humility: Measuring openness
to culturally diverse clients. Journal of Counseling Psychology, 60(3), 353–366. https://doi.org/10.1037/a0032595
Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the Working Alliance Inventory. Journal of
Counseling Psychology, 36, 223-233.
Hunt, G. E., Large, M. M., Cleary, M., Lai, H. M. X., & Saunders, J. B. (2018). Prevalence of comorbid substance use
in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: Systematic review and meta-
analysis. Drug and alcohol dependence, 191, 234–258. https://doi.org/10.1016/j.drugalcdep.2018.07.011
Jackson, C., Trower, P., Reid, I., Smith, J., Hall, M., Townend, M., Barton, K., Jones, J., Ross, K., Russell, R., Newton,
E., Dunn, G., & Birchwood, M. (2009). Improving psychological adjustment following a first episode of psychosis:
A randomised controlled trial of cognitive therapy to reduce post psychotic trauma symptoms. Behaviour and
Research Therapy, 47, 454-462.
Judge, A., Perkins, D. O., Nieri, J., & Penn, D. L. (2005). Pathways to care in first episode psychosis: A pilot study on
help-seeking precipitants and barriers to care. Journal of Mental Health, 14, 465-469.
Kane, J. M., Robinson, D. E., Schooler, N. R., Mueser, K. T., Penn, D. L., Rosenheck, R. A., Addington, J., Brunette,
M. F., Correll, C. U., Estroff, S. E., Marcy, P., Robinson, J., Lynde, D. W., Meyer-Kalos, P. S., Gottlieb, J. D.,
Glynn, S. M., Pipes, R., Kurian, B. T., Miller, A. L., Azrin, S. T., Goldstein, A. B., Severe, J. B., Lin, H., Majnu, J.,
& Heinssen, R. K. (2016). Comprehensive versus usual care for first episode psychosis: Two-year outcomes from
the NIMH RAISE Early Treatment Program. American Journal of Psychiatry, 173, 362-72
Killackey, E., Jackson, H. J., & McGorry, P. D. (2008). Vocational intervention in first episode psychosis: A
randomised controlled trial of individual placement and support versus treatment as usual. British Journal of
Psychiatry, 193, 114-120.
Kingdon, D. G., & Turkington, D. (2004). Cognitive Therapy of Schizophrenia. New York: Guilford Press.
Kurtz, M. M., & Mueser, K. T. (2008). A meta-analysis of controlled research on social skills training for
schizophrenia. Journal of Consulting and Clinical Psychology, 76, 491-504.
Lambert, M. J., Whipple, J. L., Vermeersch, D. A., Smart, D. W., Hawkins, E. J., Nielsen, S. L., & Goates, M. (2002).
Enhancing psychotherapy outcomes via providing feedback on client progress: A replication. Clinical Psychology
& Psychotherapy, 9(2), 91-103.
Lambert, M. J., Whipple, J. L., Hawkins, E. J., Vermeersch, D. A., Nielsen, S. L., & Smart, D. W. (2003). Is it time for
clinicians to routinely track patient outcome? A meta‐analysis. Clinical Psychology: Science and Practice, 10(3),
288-301.
Lewine, R. R. J. (2005). Social class of origin, lost potential, and hopelessness in schizophrenia. Schizophrenia
Research, 76, 329-335.
Lewis, C. C., Puspitasari, A., Boyd, M. R., Scott, K., Marriott, B. R., Hoffman, M., Navarro, E., & Kassab, H. (2018).
Implementing measurement based care in community mental health: A description of tailored and standardized
methods. BMC Research Notes, 11(1), 76. doi:10.1186/s13104-018-3193-0.
Liberman, R. P., Mueser, K. T., Wallace, C. J., Jacobs, H. E., Eckman, T., & Massel, H. K. (1986). Training skills in
the psychiatrically disabled: Learning coping and competence. Schizophrenia Bulletin, 12, 631-647.
Mark, T., Coffey, R., Vandivort-Warren, R., Harwood, H., & King, E. (2005). U.S. Spending for Mental Health and
Substance Abuse Treatment, 1991-2001. Health Affairs, Jan-Jun Suppl Web Exclusives, W5-133-W135-142.
McGurk, S. R., & Mueser, K. T. (2004). Cognitive functioning, symptoms, and work in supported employment: A
review and heuristic model. Schizophrenia Research, 70, 147-174.

67
Washington State New Journeys Manual – September 2023
Mihalopoulos, C., Harris, M., Henry, L., Harrigan, S., & McGorry, P. (2009). Is early intervention in psychosis cost-
effective over the long term? Schizophrenia Bulletin, 35, 909-918.
Miller, W. R., & Rollnick, S. (Eds.). (2012). Motivational Interviewing: Helping People Change (3rd ed.). New York:
Guilford Press.
Mueser, K. T., & Gingerich, S. (2006). The Complete Family Guide to Schizophrenia: Helping Your Loved One Get
the Most Out of Life. New York: Guilford Press.
Mueser, K. T., Lu, W., Rosenberg, S. D., & Wolfe, R. (2010). The trauma of psychosis: Posttraumatic stress disorder
and recent onset psychosis. Schizophrenia Research, 116, 217-227.
Mueser, K. T., Noordsy, D. L., Drake, R. E., & Fox, L. (2003). Integrated Treatment for Dual Disorders: A Guide to
Effective Practice. New York: Guilford Press.
Murray, C. J. L., & Lopez, A. D. (Eds.). (1996). The Global Burden of Disease: A Comprehensive Assessment of
Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA:
Harvard University Press.
National Institute of Mental Health. (2022, October). Recovery after an initial schizophrenia episode (RAISE).
https://www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/recovery-after-an-initial-
schizophrenia-episode-raise
Neenan, M. (2009). Developing Resilience: A Cognitive-Behavioural Approach. London: Routledge.
Nuechterlein, K. H., & Dawson, M. E. (1984). A heuristic vulnerability/stress model of schizophrenic episodes.
Schizophrenia Bulletin, 10, 300-312.
Nuechterlein, K. H., Subotnik, K. L., Turner, L. R., Ventura, J., Becker, D. R., & Drake, R. E. (2008). Individual
placement and support for individuals with recent-onset schizophrenia: Integrating supported education and
supported employment. Psychiatric Rehabilitation Journal, 31, 340-349.
Office of Disease Prevention and Health Promotion (2020). Social Determinants of Health. Retrieved
from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health#two
Oluwoye, O., Reneau, H., Stokes, B., Daughtry, R., Venuto, E., Sunbury, T., Hong, G., Lucenko, B., Stiles, B.,
McPherson, S.M. and Kopelovich, S., Monroe-DeVita, M., & McDonell, M. G. (2020). Preliminary evaluation of
Washington state’s early intervention program for first-episode psychosis. Psychiatric Services, 71(3), 228-235.
Penn, D. L., Waldheter, E. J., Mueser, K. T., Perkins, D. O., & Lieberman, J. A. (2005). Psychosocial treatment for
first episode psychosis: A research update. American Journal of Psychiatry, 162, 2220-2232.
Perkins, D. O., Gu, H., Boteva, K., & Lieberman, J. A. (2005). Relationship between duration of untreated psychosis
and outcome in first-episode schizophrenia: A critical review and meta-analysis. American Journal of Psychiatry,
162, 17851804.
Perry, B. M., Taylor, D., & Shaw, S. K. (2007). "You've got to have a positive state of mind": An interpretative
phenomenological analysis of hope and first episode psychosis. Journal of Mental Health, 16, 781-793.
Petersen, L., Jeppesen, P., Thorup, A., Abel, M. B., Ohlenschlager, J., Christensen, T. O., Krarup, G., Jorgensen, P., &
Nordentoft, M. (2005). A randomized, multicenter trial of integrated versus standard treatment for patients with a
first episode of psychotic illness. British Medical Journal, 331, 602-609.
Power, P. (2004). Suicide prevention in early psychosis. In J. Gleeson & P. D. McGorry (Eds.), Psychological
Interventions in Early Psychosis: A Treatment Handbook (pp. 175-190). Chichester, England: John Wiley & Sons.
President's New Freedom Commission on Mental Health. (2003). Achieving the Promise: Transforming Mental Health
Care in America: Final Report (DHHS Pub. No. SMA-03-3832). Rockville, MD: Substance Abuse and Mental
Health Services Administration.
Rapp, C. A., & Goscha, R. J. (2006). The Strengths Model: Case Management with People with Psychiatric
Disabilities (Second ed.). New York: Oxford University Press.
Robinson, D., Woerner, M. G., Alvir, J. M., Bilder, R., Goldman, R., Geisler, S., Koreen, A., Sheitman, B., Chakos,
M., Mayerhoff, D., & Lieberman, J. A. (1999). Predictors of relapse following response from a first episode of
schizophrenia or schizoaffective disorder. Archives of General Psychiatry, 56, 241-247.
Ryff, C. D., & Singer, B. (1998). The contours of positive human health. Psychological Inquiry, 9, 1-28.

68
Washington State New Journeys Manual – September 2023
Samnaliev, M., & Clark, R. E. (2008). The economics of schizophrenia. In K. T. Mueser & D. V. Jeste (Eds.), Clinical
Handbook of Schizophrenia (pp. 507-515). New York: Guilford Press.
Teplin, L. A. (1994). Psychiatric and substance abuse disorders among male urban jail detainees. American Journal of
Public Health, 84, 290-293.
Teplin, L. A., Abram, K. M., & McClelland, G. M. (1996). Prevalence of psychiatric disorders among incarcerated
women. I. Pretrial jail detainees. Archives of General Psychiatry, 53, 505-512.
Towle, A., & Godolphin, W. (1999). Framework for teaching and learning informed shared decision making. British
Medical Journal, 319, 766-771.
Uzenoff, S. R., Perkins, D. O., Hamer, R. M., Wiesen, C. A., & Penn, D. L. (2008). A preliminary trial of adherence-
coping-education (ACE) therapy for early psychosis. Journal of Nervous and Mental Disease, 196, 572-575.
Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., Read, J., van Os, J., & Bentall, R. P.
(2012). Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and
cross-sectional cohort studies. Schizophrenia bulletin, 38(4), 661–671. https://doi.org/10.1093/schbul/sbs050
Weiss, A., Steadman, S., Mercier, H.D, Hansel, T.C., Chaudhry, S., & Clark, I. Pathways to Care: How Help-Seeking
Behaviors Relate to Duration of Untreated Psychosis and Treatment Engagement. Psychiatric Quarterly, 93, 473–
482 (2022). https://doi.org/10.1007/s11126-021-09960-5
Williams-Keeler, L., Milliken, H., & Jones, B. (1994). Psychosis as precipitating trauma for PTSD: A treatment
strategy. American Journal of Orthopsychiatry, 64, 493498.
Zubin, J., & Spring, B. (1977). Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology, 86, 103-
126.

69
Washington State New Journeys Manual – September 2023
GLOSSARY OF TERMS
Attestation – An attested provider refers to a team that has completed the start-up phase and is recognized by the New
Journeys network as having completed the necessary training to provide New Journeys services. Attested teams are also
ready to accept referrals. New Journeys teams typically become attested at the end of the first year of startup and case
building. An attestation form is completed and submitted to HCA documenting that basic training, staffing and fidelity
requirements have been met.
Case Building – The process of completing intake for 2-3 participants per month, working towards a case load of 30
enrollees over time. Developing a caseload in this way accounts for the additional time needed for staff training and a
higher level of service intensity during the initial months of an individual’s participation in New Journeys.
Case Building Funds – Per the fidelity model, new NJ teams are required to “ramp up” their caseloads incrementally
over time, as required by legislation and guidelines. A full team takes between 15 and 24 months to reach full capacity.
“Case building funds” are included in the provider or BH-ASO contracts with DBHR to supplement the New Journeys
teams while they are working toward a full caseload.
Coordinated Specialty Care (CSC) – A recovery-oriented, team approach to treating early psychosis that promotes easy
access to care and shared decision-making among specialists, the person experiencing psychosis, and family members.
Specifically, coordinated specialty care involves multiple components: Individual or group psychotherapy, family support
and education, medication management, supported employment and education,
and case management.
Community Launch – An agency’s readiness to begin accepting referrals for the New Journeys team from outside of the
agency. These referrals will be generated through the marketing, education, and outreach efforts to provide education to
the community about the availability of New Journeys services in the area.
Division of Behavioral Health and Recovery (DBHR) – The HCA-designated state mental health authority that is
tasked with administering the state- and Medicaid-funded mental health programs authorized by the Revised Code of
Washington chapters 71.05, 71.24, and 71.34.
Duration of Untreated Psychosis (DUP) – The time between the onset of psychotic symptoms and the initiation of
treatment.
Family Education Provider – A master’s level team member who helps an individual’s natural supports learn about
psychosis and its treatment while developing strategies for coping with stress and communicating effectively. This team
member is sometimes also referred to as a Family Education Provider, Family Education Specialist, or simply Family
Educator and is often a shared role with the Program Director.
Fidelity Monitoring – The system of measuring and evaluating the degree to which the model is implemented as
intended. Fidelity to the New Journeys model is measured through annual site visits with DBHR during the startup and
case building phase, and/or through the University of Washington (UW) Fidelity Review Process beginning in year 2 of
implementation. Fidelity to the data-driven and measurement elements and use of the data delivery platform are
continuously monitored for fidelity by the Washington State University (WSU) Measurement and Evaluation team.
First Episode Psychosis (FEP) – The time period when a person first shows signs of perceptual changes and loss of
contact with reality (typically within one week to two years from the onset of changes). The longer symptoms of
psychosis go untreated, the more severe and chronic symptoms become, resulting in decreased functioning and other

70
Washington State New Journeys Manual – September 2023
negative outcomes over the course of their lifetime. The goal of addressing FEP within the first two years of onset is to
improve outcomes throughout an individual’s lifetime.
Implementation Team – The University of Washington Training and Consultation Team
Individual Resiliency Training Therapist – The team’s master’s level therapist who provides Cognitive Behavioral
Therapy for psychosis (CBTp). This team member provides culturally competent, trauma-informed, strengths-based, and
measurement-based care for participants enrolled on the New Journeys team. The team member is sometimes referred to
as the IRT Therapist, IRT Clinician, IRT Specialist, or simply IRT.
Natural Supports – A source of support that comes directly from people and communities rather than through paid forms
of support. These may include family, chosen family, friends, school classmates, work colleagues, or other community
supports.
New Journeys Measurement Battery- a set of standardized assessment tools or instruments used to evaluate various
aspects of an individual's mental health and functioning when receiving comprehensive and evidence-based early
intervention and treatment for individuals experiencing their first episode of psychosis. This tool collects information
about the key domains of early psychosis symptoms, recovery, and treatment to facilitate measurement-based early
psychosis care and research.
New Journeys or the New Journeys Model – An evidenced-informed, CSC treatment model for older youth and young
adults who are experiencing FEP. New Journeys is more intensive than regular outpatient services and is curated
specifically to meet the needs of those in the early stages of psychosis. Treatment goals focus on functional recovery and
are defined by what is meaningful to the youth and their family. Routine outcome monitoring or measurement-based care
is utilized by teams throughout care to inform youth and families of progress, improve outcomes, and to drive practice
improvements.
New Journey’s Manual – Document that provides guidelines to ensure consistency in the goals, principles, and delivery
of New Journeys services across Washington State.
New Journeys Team – The professional team providing New Journeys services. This team is expected to be comprised of
a Program Director/Family Education Specialist (1.0 FTE), a Psychiatrist or Advanced Registered Nurse Practitioner
(ARNP) (0.25 FTE), an Individual Resiliency Therapist (1.0 FTE), a Supported Employment and Education Specialist
(1.0 FTE), a Case Manager (0.5 FTE), and a Peer Specialist (0.5 FTE) with total FTE count of 4.25. Teams may choose to
substitute a Nurse Care Manager (~0.2 FTE) for all or part of the case manager FTE count. Exceptions to this team
staffing composition must be approved in writing by DBHR. A full fidelity team serves up to 30 individuals with FEP
who meet eligibility criteria for New Journeys. Team members are expected to engage in ongoing training/consultation
with UW and WSU. A fully functioning New Journeys team has submitted a New Journeys Attestation which has been
approved by DBHR.
Measurement and Evaluation Team – The network supports at Washington State University who implement the New
Journeys data platform.
Measurement-Informed Care – The use of standardized measures to guide treatment practice or treatment planning.
Nurse Care Manager – A registered nurse who has dedicated time within an agency to support New Journeys
participants. This team member focuses on supporting healthy behaviors, wellness, and care coordination. This team
member is often referred to as the nurse or RN.
71
Washington State New Journeys Manual – September 2023
Mental Health Block Grant (MHBG) – The funds granted to states by the Secretary of the DHHS through the Center for
Mental Health Services (CMHS) and the Substance Abuse and Mental Health Services Administration (SAMHSA) to
establish or expand an organized community-based system for providing mental health services for adults with SMI and
children with Severe Emotional Disturbance (SED). States must submit an application in accordance with the law for
applicable fiscal years for which they seek MHBG funds. Awarded MHBG funds must be used to: a) carry out the State
plan contained within the application, b) evaluate programs and services set in place under the plan, and c) conduct
planning, administration, and educational activities related to the provision of services under the plan.
Peer Reviewers – Describes New Journeys Team Members who have been trained in/participate in the fidelity review
process as co-reviewers with UW.
Peer Support Specialist – A member of the team who has lived experience with mental health challenges and has
completed training in the Washington State Certified Peer Counselor Training Program. This team member assists with
engagement of individuals experiencing psychosis in services throughout treatment to ensure that they have the
information and resources they need to direct their treatment and to use an empowered voice in the treatment planning
process. This team member is often referred to as the Peer Specialist or simply the Peer.
Program – Refers to implementation of the New Journeys Model
Program Director – A master’s level clinician who serves as the New Journeys clinical team lead. This team member
monitors and oversees all team operations, leads regular team clinical meetings, supervises the other team clinicians, is
responsible for outreach and community education (community relations), develops a strong referral network within the
agency and region, and leads the screening process for referrals. This is often a shared role with the Family Education
Provider.
Psychiatric Care Provider – A Psychiatrist or a Psychiatric Advanced Registered Nurse Practitioner (ARNP) who is
responsible for psychiatric diagnosis, medication management for psychiatric and substance use disorders, acute
management of suicidality and safety concerns, and physical health care needs in coordination with the team nurse and
primary care provider.
REDCap – The database currently in place as the New Journeys measurement-based care delivery and data platform.
SAMHSA – The U.S. Department of Health and Human Services Substance Abuse and Mental Health Services
Administration.
Severe Emotional Disturbance/Severe Mental Illness or SED/SMI – Children from birth to age 18 (SED) and adults
age 18 and over (SMI): (1) who currently meet or at any time during the past year has met criteria for a mental disorder –
including within developmental and cultural contexts – as specified within a recognized diagnostic classification system
(e.g., most recent editions of DSM, ICD, etc.), and (2) who displays functional impairment, as determined by a
standardized measure, which impedes progress towards recovery and substantially interferes with or limits the person’s
role or functioning in family, school, employment, relationships, or community activities.
Soft Launch – Describes an agencies readiness to begin accepting referrals for the New Journeys team from withing the
agency. These referrals have been identified as potential candidates for the New Journeys team through the education and
training provided by the Program Director within the agency.
Startup Funds – Funding for newly established New Journeys teams provided through contracts with DBHR before the
team provides any services. This may include capital and training expenditure funds.

72
Washington State New Journeys Manual – September 2023
Supported Education and Employment Specialist – An experienced bachelor’s or master’s level clinician who works
from a recovery orientation and focuses on assisting individuals experiencing psychosis to achieve recovery goals related
to education and employment. This team member is often referred to as the SEE or SEE Specialist.
Team Based Rate (TBR) – The two-tiered Medicaid service-based enhancement financial model developed though an
actuarial process. The tiers reflect a higher level of service intensity during the first six months of treatment. The service-
based enhancement is paid to the Managed Care Organizations as a Per User Per Month (PUPM) payment. The fiscal
assumptions supporting the PUPM amount fully supports the costs of the NJ teams to provide this service to Medicaid
enrollees. Enrollees will be eligible for the New Journeys Team Based Rate for a duration of up to 24 months of
treatment. The New Journeys contractor will serve individuals with Medicaid coverage as well as facilitate 2 non-
Medicaid slots funded through the regions BH-ASO.

73
Washington State New Journeys Manual – September 2023
APPENDIX A: EXAMPLE JOB DESCRIPTIONS
Program Director and Family Education Provider
TITLE: New Journeys Program Director and Family Education Provider
GENERAL FUNCTION:
The ideal candidate for the program director/family education specialist is a licensed clinician with experience in
diagnostic screening and assessment of psychotic disorders, expertise working with individuals with schizophrenia-
spectrum disorders and their families utilizing evidence-based practices such as multi-family groups, and experience
connecting families with an array of self-help tools and resources.
The program director monitors and oversees all team operations, leads regular team clinical meetings, and supervises the
other team clinicians. The program director is responsible for outreach and recruitment in the community, develops strong
referral sources, and leads the screening process for referrals. They are the primary contact person for clients and families,
and spearhead efforts to engage clients in treatment. They work with individuals and their families, providing education
about psychosis and how to manage it, improving communication and problem-solving skills, and encouraging a
strengths-based, recovery-oriented approach to psychosis. The program director works with participants and families
using a shared decision-making process.
RESPONSIBLE TO: Director of Outpatient Programming
QUALIFICATIONS:
• Master’s degree in Psychology, Social Work or closely related field with accepted licensure and preferred
experience as a Clinical Supervisor.
• Experience providing mental health services to individuals experiencing SED/SMI
• Knowledge of and experience with developmental and treatment strategies towards current DSM covered
diagnoses.
• Knowledge of and experience with the community support model.
• Previous experience working as a member of a multidisciplinary treatment team and experience working
collaboratively with other service providers.
• Relevant therapeutic skills.
• Strong interpersonal skills.
• Strong organizational skills including the use of electronic medical record software or equivalent for scheduling,
time management and all clinical documentation.
• Must pass a criminal background and Inspector General check.
DUTIES AND RESPONSIBILITIES:
Direct the day-to-day clinical operations of the care team, and provide administrative coordination as needed with
referral sources.
• Assure that the quality of care provided meets fidelity standards provided for the statewide network of New
Journeys care teams.
• Participate in the comprehensive assessment of client needs to assure person-centered treatment planning.
• Work with clients and their families, providing education about psychosis and how to manage it, improving
communication and problem-solving skills.

74
Washington State New Journeys Manual – September 2023
• Oversee data collection through clinical tools and protocols designed to measure key indicators of progress in
treatment for this population.
• Assist clinicians with the performance of their duties by overseeing and participating in clinical
coordination/problem solving between clients and clinicians and other agency programs and community
resources. Coordinate crisis intervention with the Crisis Response team, Crisis Triage Center, and other providers
as clinically necessary.
• Participate in monthly training provided by Washington Health Care Authority First Episode Psychosis Program,
Washington State University, and the University of Washington. Consult with their program director trainer and
receive support for program development as your team starts serving clients.
• Maintain a trauma-informed work environment with a focus on the utilization of Recovery-Based Language in
both written and verbal communications.

75
Washington State New Journeys Manual – September 2023
Individual Resiliency Training Therapist (IRT)
TITLE: New Journeys Individual Resiliency Training (IRT) Clinician
GENERAL FUNCTION:
New Journeys is a coordinated specialty care team that uses evidence-based treatment to provide intensive services to up
to 30 individuals aged 15-40 experiencing their first episode of psychosis.
The New Journeys Program Individual Resiliency Trainer (IRT) clinician is a recovery-oriented, experienced master’s
level clinician who provides evidence-based therapeutic services in a managed care environment to transitional age youth
or adults and their families. They assist clients to identify and developing recovery goals, learn about psychosis and skills
for managing it, develop coping skills for stressful situations and persistent symptoms, and address challenges related to
achieving their recovery goals. It is desirable (but not required) that the IRT clinician have a background in Cognitive
Behavioral Therapy (CBT) skills, such as social skills training, cognitive restructuring, behavioral activation, coping skills
training, relaxation training, and psychoeducation. Experience with adolescents and young adults is an advantage, but not
required.
An IRT clinician must have the ability to meet with individuals outside of typical 8am-5pm work hours and have the
capacity to make home and community visits.
RESPONSIBLE TO: New Journeys Program Director
QUALIFICATIONS:
• Master’s degree in Psychology, Social Work or closely related field with accepted licensure or eligible for
supervision towards agency accepted licensure.
• Experience in providing mental health services to severely emotionally disturbed children, adolescents, and
families.
• Knowledge and experience with developmental and treatment strategies towards current DSM covered diagnosis.
• Demonstrated ability to provide culturally competent treatment services to diverse client populations and maintain
a cooperative working relationship with others in a culturally diverse environment
• Must have a strong commitment to the right and the ability of each person with a severe mental illness to live in
normal community residences; work in market jobs; and have access to helpful, adequate, competent, and
continuous supports and services.
• Knowledge of and experience with the community support model.
• Previous experience working as a member of a multidisciplinary treatment team and working collaboratively with
other service providers.
• Relevant therapeutic skills.
• Strong interpersonal skills.
• Strong organizational skills including the use of electronic medical record software or equivalent for scheduling,
time management and all clinical documentation.
• Must pass a criminal background and Inspector General check.
TYPICAL DUTIES & RESPONSIBILITIES:
• Work in collaboration with referral sources, community service providers, and adjunctive service providers to
assess, develop and facilitate individualized treatment services and ensure continuity of care.
• Provide a broad range of medically necessary therapeutic services, including intakes within the framework of a
community support model. Services may be provided in agency sites, school, homes and other appropriately
deemed community settings.

76
Washington State New Journeys Manual – September 2023
• Work collaboratively with multi-disciplinary team. Manage individual and shared client caseloads per agency
guidelines, develop services appropriate to a community-based service model, and participate in the management
of program resources within a managed care framework. Emphasis of caseload will be on youth presenting with
early episode psychosis issues and treatment thereof.
• Work in collaboration with other clinicians, leadership, and referral sources to assess, develop, and facilitate
individual client treatment services and ensure consistency of care with other involved providers.
• Develop 24-hour crisis plans for assigned youth and utilize the High Risk Protocol as appropriate.
• Maintain client’s chart in accordance with WAC and agency standards. Adhere to agency policy pertaining to
documentation and chart maintenance.
• Participate in clinical supervision and psychiatric consultation on a regular and scheduled basis.
• Attend mandatory meetings as assigned.
• Adhere to agency Performance Standard Expectations.
• Maintain contact with utilization review team regarding authorizations and funding for services.
• Practice successful client engagement skills and strategically address clients with a frequent and predictable no-
show pattern. Close clients when appropriate.
• Maintain regular attendance in order to ensure continuity of quality client care.
• Other duties as needed to fulfill the goals of the New Journeys program including blended roles while building
toward capacity.
• Maintain the New Journeys evidence/research-based fidelity model while delivering services.

77
Washington State New Journeys Manual – September 2023
Supported Education and Employment Specialist
TITLE: New Journeys Supported Education and Employment (SEE) Specialist
GENERAL FUNCTION:
The New Journeys Supported Education and Employment (SEE) Specialist provides a range of community-based
vocational and educational support services.
New Journeys is a coordinated specialty care team that uses evidence-based treatment to provide intensive services to up
to 30 individuals aged 15-40 experiencing their first episode of psychosis. A potential candidate for this position should
have prior experience as a supported education specialist, supported employment specialist, vocational specialist, and/or
an intensive case manager. Because of the nature of this job, SEE Specialists need to work directly in the community with
employers, potential employers, educational personnel, and families. They connect with community partners and families
and spend the majority of their time out of the office providing direct services to clients.
PURPOSE: Assesses participants for employment and/or education goals/capabilities/needs, provides training assistance,
and offers continuing support. Assists clients in targeting potential jobs and/or education, exploring job and/or education
possibilities in the community, and making job and/or education placements. They work with participants and families
using a shared decision-making process. Adjunctive services may include issue-specific and psycho-educational groups,
in-home behavioral skills enhancement, and coordination of systems of care. A vital part of this position is community
education with employers and community providers about the agency’s New Journeys Program and how they operate as a
successful community support model for employing people with behavioral health challenges. This includes encouraging
them to recognize individuals' abilities to be productive and successful. Services are offered in a community, school, and
home-based settings.
RESPONSIBLE TO: New Journeys Program Director
QUALIFICATIONS:
• Bachelor’s degree in Psychology, Social Work or closely related field with agency accepted licensure or eligible
for supervision towards BHR accepted licensure.
• Experience developing community-based employment and/or education opportunities
• Must have at least one year of documented experience working with individuals with disabilities or one year of
human service-related experience addressing issues such as economic disadvantages, employment, abuse and
neglect, substance abuse, aging, disabilities, prevention, health, cultural competencies, or housing
• Must have a strong commitment to the right and the ability of each person with a severe mental illness to live in
normal community residences; work in market jobs; and have access to helpful, adequate, competent, and
continuous supports and services.
• Bilingual (Spanish/English) fluency skills preferred but not required
• Previous experience working as a member of a multi-disciplinary team
• Knowledge of and experience with the community support model
• Demonstrated ability to provide culturally competent treatment services to diverse client populations and maintain
a cooperative working relationship with others in a culturally diverse environment
• Ability to provide employment and/or education services and compliance with confidentiality in accordance with
federal, state, and/or funding source requirements
• Knowledge of community resources to enable appropriate referrals for specific client needs
• Proficient in Microsoft Outlook, Excel, and Word; ability to master proprietary software including electronic
health record system required

78
Washington State New Journeys Manual – September 2023
• Access to a car, a valid driver's license, proof of current automobile insurance coverage, and ability to meet the
agency’s driving requirements
• Must pass a criminal background and Inspector General check
TYPICAL DUTIES & RESPONSIBILITIES:
• Interviews individuals and, if applicable, family members or team members in the client support system to
complete the strengths-based vocational/educational assessment to identify clients' skills and strengths, interests,
goals, dreams, aspirations, and resources available to reach their goals.
• Provides counseling to individuals to help them understand and overcome personal, social, or behavioral
problems affecting their vocational/educational situations.
• Develops an employment and/or education focused service plans based on clients' interests, abilities, strengths
and needs; service plans will be client driven and follow-ups will be completed on time, assessing the quantity
and quality of services provided.
• Researches possible job and/or education openings and opportunities for clients by contacting employment/school
services, newspaper want ads, previous contacts, cold calling, and any other means of reaching potential
employers and/or schools.
• Performs job analyses, matching potential openings with clients' needs, skills, and logistics of getting to the job
site.
• Establishes and maintains connections with businesses offering employment opportunities.
• Sets up interviews for clients, assists clients with applications, resume preparation, and interviewing skills.
• Locates barriers to client employment and/or educational goals, such as inaccessible sites, inflexible schedules,
finances, and transportation problems, and works with clients to develop strategies for overcoming these barriers.
• Maintains close contact with clients during job and educational placements to resolve problems and evaluate
placement adequacy.
• Performs interventions as needed with assigned clients previously placed who may be at risk of losing their jobs
and/or education.
• Coordinates and consults with other team members to keep the team informed of issues and progress
• Provides counseling to individuals, groups, families, or communities regarding vocational and educational
rehabilitation issues.
• Participates in clinical supervision, team consultation, and psychiatric consultation on a weekly basis.
• Participates in monthly consultation calls with the UW New Journeys training team.
• Attends all team meetings including business meetings and case reviews; attend individual service team meetings
as negotiated with treatment team.
• Maintains clients’ charts in accordance with WAC and agency standards; adhere to agency policy pertaining to
documentation, chart maintenance, and other required paperwork.
• Works collaboratively with agency and New Journeys multi-disciplinary teams; manage individual and shared
client caseloads per agency guidelines, develop services appropriate to a community-based service model, and
participate in the management of program resources within a managed care framework.
• Transports clients in a personal vehicle.
• Other duties as needed to fulfill the goals of the New Journeys Program.
PHYSICAL REQUIREMENTS:
• Ability to perform essential duties of the position
• Ability to travel to other sites is required
• Ability to look at and use a computer for extended periods of time
• Work is performed in an office and in the community; sufficient mobility to meet with other employees and
attend meetings at various locations is required
• Requires periods of intense concentration over extended period of time, and is subject to frequent interruption

79
Washington State New Journeys Manual – September 2023
• Ability to access locations that are not ADA accessible
• Ability to work with individuals in a variety of locations to include office, schools, homes, and community
• Possess a current WA state driver’s license and reliable transportation

80
Washington State New Journeys Manual – September 2023
Peer Support Specialist
TITLE: New Journeys Peer Support Specialist
GENERAL FUNCTION:
This member of the team has experience as a recipient of mental health services for severe and persistent mental illness
and is willing to share his or her personal, practical experience, knowledge, and first-hand insight to benefit the team and
its clients. The Peer Support Specialist provides expertise about the recovery process, symptom management, and the
persistence required to encourage clients to reach their goals. They collaborate to promote a team culture that recognizes,
understands, and respects each client’s point of view, experiences, and preferences. They are responsible for maximizing
client choice, self-determination and decision making in the planning, delivery and evaluation of treatment, rehabilitation,
and support services. They provide peer counseling for New Journeys first episode psychosis clients. This includes
carrying out rehabilitation and support functions and assisting in treatment, education, and crisis intervention under the
clinical supervision of staff with professional degrees.
RESPONSIBLE TO: New Journeys Program Director
QUALIFICATIONS:
• A high school diploma is required and two years of paid or volunteer work experience with youth and/or adults
with mental illness is highly desired.
• Completed Peer Certification Training with proof of completion is required.
• Must have good oral and written communication skills.
• The Peer Support Specialist, who is or has been a recipient of mental health services for severe and persistent
mental illness or severe emotional disturbance, should have the self-knowledge needed to manage their mental
illness and be well along in their recovery.
• Must have a strong commitment to the right and the ability of each person with a severe mental illness to live in
normal community residences; work in market jobs; and have access to helpful, adequate, competent, and
continuous supports and services.
• Demonstrated ability to provide culturally competent treatment services to diverse client populations and maintain
a cooperative working relationship with others in a culturally diverse environment
• It is essential the Peer Support Specialist has skills and competence to establish supportive trusting relationships
with youth and young adults with SMI/SED and respect for clients' rights and personal preferences in treatment is
essential.
• Able to demonstrate initiative and success in providing client-centered interaction, solution-based approaches to
learning, motivation techniques and positive reinforcement skills.
• Able to demonstrate patience, creative thinking, good decision-making skills, and a willingness to assist clients
with achieving treatment plan goals.
• Able to demonstrate the ability to maintain appropriate professional boundaries while teaching necessary living
skills to clients.
• Demonstrates ability to be organized and keep accurate and timely records.
• Demonstrates an ability to work independently and as a positive team player.
• Demonstrates good time management skills.
• Requires a valid WA State driver's license and use of own vehicle with BHR approved insurance.
TYPICAL DUTIES &
RESPONSIBILITIES:
• Meets regularly as scheduled with New Journeys team to receive work assignments.

81
Washington State New Journeys Manual – September 2023
• Writes and submits progress notes for each client seen on each day of service. Progress notes must meet the
standards of content and legibility set for the program.
• Organizes and schedules work time in order to complete assignments and all related paperwork in a timely
manner and according to program standards.
• Attends required program and agency trainings.
• Attends ongoing briefing and debriefing consultations as are relevant to the program.
• Meets with Supervisor on a regular basis as scheduled. Accepts direction and carries out self-care methods to stay
healthy.
• Acts as an interpreter to help non-mental health consumer team members better understand and empathize with
each client’s unique and subjective experience and perceptions.
• Provides expertise and consultation from a mental health consumer perspective to the entire team concerning
client’s experiences on symptoms of mental illness, the effects and side effects of medications, clients’ responses
to opinions of treatment and clients’ experience of recovery.
• Collaborates with the team to promote a team culture in which each client’s point of view, experiences, and
preferences are recognized, understood, and respected, and in which client self-determination and decision
making in treatment planning are maximized and supported.
• Helps clients identify, understand and combat stigma and discrimination associated with mental illness and
develop strategies to reduce self-stigma.
• Helps other team members identify and understand culture-wide stigma and discrimination against people with
mental illness and develop strategies to eliminate stigma within the team.
• Helps clients develop interests and personal identity outside of the mental health system.
• Other duties as assigned to meet necessary goals of the position.
PHYSICAL REQUIREMENTS:
• Must be able to drive and to transport clients as needed.
• Ability to work in office, home, school, and community-based settings.
82
Washington State New Journeys Manual – September 2023
APPENDIX B: RECURRING TRAINING AND CONSULTATION HOURS FOR NEW
JOURNEYS TEAM MEMBERS
Trainings
Program
Director/
Family Ed.
Specialist
Family Ed.
Specialist
(only)
IRT
Clinician
SEE
Specialist
Peer
Psychiatric
Care
Provider
Nurse
Care
Manager
Consultation
Calls
36 Hours
(Prog Dir =
12 hrs
Family Ed =
12 hrs
Diff Dx = 12
hrs)
12 Hours
12 – 24
Hours
(IRT = 12
hrs
*Diff Dx =
12 hrs)
12 Hours
12
Hours
12 Hours
12 Hours
ECHO
18 Hours
(12 clinics x
90 min)
18 Hours
(12 clinics x
90 min)
18 Hours
(12 clinics
x 90 min)
18 Hours
(12 clinics x
90 min)
18
Hours
(12
clinics x
90 min)
18 Hours
(12 clinics x
90 min)
18 Hours
(12 clinics
x 90 min)
Start-Up
16 Hours
(8 hrs x 2
days)
16 Hours
(8 hrs x 2
days)
16 Hours
(8 hrs x 2
days)
16 Hours
(8 hrs x 2
days)
16
Hours
(8 hrs x
2 days)
8 Hours
(8 hrs x 1 day)
8 Hours
(8 hrs x 1
day)
One specialty
topic
8 Hours
(8 hrs x 1
days)
8 Hours
(8 hrs x 1
days)
8 Hours
(8 hrs x 1
days)
8 Hours
(8 hrs x 1
days)
8 Hours
(8 hrs x
1 days)
8 Hours
(8 hrs x 1
days)
8 Hours
(8 hrs x 1
days)
Fidelity review
preparation
and
participation
18 Hours
N/A
N/A
N/A
N/A
N/A
N/A
REDCap
training
6 Hours
(4 hrs x 1
day
+ 1 hr x 2
days)
6 Hours
(4 hrs x 1 day
+ 1 hr x 2
days)
6 Hours
(4 hrs x 1
day
+ 1 hr x 2
days)
6 Hours
(4 hrs x 1
day
+ 1 hr x 2
days)
6 Hours
(4 hrs x
1 day
+ 1 hr x
2 days)
6 Hours
(4 hrs x 1 day
+ 1 hr x 2
days)
6 Hours
(4 hrs x 1
day
+ 1 hr x 2
days)
Total Annual
Training
Hours
102 Hours
60 Hours
60-72
Hours
60 Hours
60
Hours
52 Hours
52 Hours

83
Washington State New Journeys Manual – September 2023
APPENDIX C: EXAMPLE OF AGENCY LEVEL NEW JOURNEY’S FLOW SHEET
Purpose
This purpose of this protocol is to clearly define the process for accepting new clients into the New Journey’s program
within an agency. Any specific questions related to New Journey’s clients and the admission process should be directed to
the appropriate New Journey’s supervisor.
Protocol
External Referrals
I. New Journeys staff receive a request for information or referral for an individual not currently enrolled in
services at the agency.
II. New Journeys staff will request Office Support (OS) open a chart for potential client in the Electronic Health
Record under the New Journeys-Request for Services (NJ-RFS) program.
III. OS staff will open the RFS episode by completing the following:
A. Checking Provider One for Medicaid coverage
B. Consumer First Contact Service form
C. Admission form
D. Please note: OS will enter an Admission Diagnosis of R69 for the same date and time Episode was opened
(Type of Diagnosis = Admission, Assessment Type = Admission).
IV. New Journeys staff will obtain funding information for the potential client
A. New Journeys staff will ask client/guardian if client has additional funding/insurance coverage
1. If client has private insurance, staff will make a copy of front and back of insurance card and submit for
scanning
B. New Journey’s staff will email all funding information to the agency Financial Department
V. New Journeys staff will bill to, and document contact with, client and collaterals in the Electronic Health Record
in the NJ-RFS Episode, using the allowable codes:
A. SAC (H0023HW) “Engagement + Outreach” for face-to-face service
B. SAC (H0023HWGQ) “Engagement + Outreach –Phone” for phone service
C. Specify in each note that you are working on assessment and engagement
D. For related travel, staff will use SAC (735) “Travel”
VI. If New Journeys staff decides client is not appropriate for New Journeys during the engagement/screening
process:
A. New Journey’s staff will complete Discharge Summary form
B. After finalizing Discharge Summary form, New Journey’s supervisor will complete Discharge form – Type of
Discharge is “OP – Terminated by Facility,” Note is “Not appropriate for New Journeys – Referred to ”
C. Clients with Medicaid coverage or those who wish to pay out of pocket should be referred to the agency for
walk-in intake assessment, or other appropriate community partner (ex. WISe).
D. Clients with private insurance should be referred to provider who accepts client’s funding source

84
Washington State New Journeys Manual – September 2023
VII. If New Journeys staff decides client might be appropriate for New Journeys during the engagement/screening
process, and the client agrees to complete Intake:
A. New Journeys staff will provide OS with information about when the Intake Assessment can be completed.
B. OS will make an appointment in the Electronic Health Record Scheduling Calendar.
VIII. If the client does show up for their scheduled intake:
A. New Journeys staff will enter a Program Transfer from NJ-RFS to the New Journeys program.
B. New Journeys staff will complete agency paperwork, Agency Intake Assessment including Diagnosis (Type
of Diagnosis = Update, Assessment Type = At Admission), and New Journeys specific assessments with
client. The Intake should be billed to and documented in the New Journeys episode using the following codes:
1. Full/completed intake: SAC (90791) “Diagnostic Evaluation-No Medical”
2. Unfinished intake (part 1) SAC (9079153) “Diag Eval-Not Completed”
3. Unfinished intake (part 2): SAC (9079152) “Diag Eval –Abrv, Partl or Update”
C. New Journeys staff will complete the agency Authorization form.
1. For clients who will be admitted to New Journeys, Authorization Type is New Journeys.
D. New Journeys staff will submit all agency paperwork to OS for processing
E. Once all documentation, including intake, is submitted for clients who will be served in New Journeys, New
Journeys staff can begin using all approved Service Activity Codes.
F. All services for admitted New Journeys clients should be billed to and documented in the New Journeys
episode.
IX. If the client does not show up for their intake appointment:
A. New Journeys staff will call client or hospital and explain they missed their scheduled appointment and either
inform the client of agency’s walk-in intake hours or attempt to schedule a new intake.
1. Bill phone service as SAC (H0023HWGQ) “Engagement + Outreach –Phone”
B. New Journeys staff will complete Discharge Summary form
C. After finalizing Discharge Summary form, New Journey’s supervisor will complete Discharge form – Type of
Discharge is “OP – Terminated by Facility,” Note is “Client did not show for Intake”
Internal Referrals
X. The New Journeys Supervisor will consult with the agency staff requesting admission into New Journeys to
confirm that the client meets eligibility for screening.
XI. If it is agreed that the client meets eligibility criteria, and the client is agreeable to completing a screening, New
Journeys staff will open a NJ-RFS episode in the Electronic Health Record.
XII. Please Note: If a client is being referred from intake and has not yet started services with New Journeys and is
eligible for New Journeys, a NJ-RFS does not need to be opened and screening will be completed under the OP
episode. Each potential New Journeys client that is being referred internally should be individually evaluated as to
whether or not a NJ-RFS episode should be opened. As a general rule of thumb: If the client clearly meets criteria
for New Journeys, and is agreeable to participate in the program, the client can be immediately enrolled in the
New Journeys program – thus bypassing the NJ-RFS episode.
XIII. If more time is needed to determine client eligibility, and for client engagement and outreach, a NJ-RFS episode
should be opened. If this is done, a new Consumer First Contact Service form must also be created.

85
Washington State New Journeys Manual – September 2023
XIV. If New Journeys staff meets with client and/or collaterals without the regular Attending Practitioner, bill to and
document under the new NJ-RFS episode.
XV. If New Journeys staff meets with client and/or collaterals with Attending Practitioner, bill to and document in the
new NJ-RFS episode using the following code:
A. SAC (22) “Secondary Practitioner”
XVI. If client is not appropriate for New Journeys, this should be documented in client chart under the new NJ-RFS
episode. Once documented, and all parties notified, the NJ-RFS episode may be closed.
XVII. If the New Journeys staff decides client will be appropriate for New Journeys during the engagement/screening
process, and the client agrees to engage in the New Journeys program:
A. New Journeys Supervisor will enter a Program Transfer to New Journeys program.
B. New Journeys Supervisor will ensure that a new agency Authorization form is completed that states the new
program for the client. Authorization Type is “New Journeys”.
XVIII. Once all documentation is submitted for clients who will be served in New Journeys, New Journeys staff can
begin using all approved Service Activity Codes.
XIX. All services for admitted New Journeys clients should be billed to and documented in the New Journeys episode.
XX. Please Note: For internal clients moving into the New Journeys program, the New Journeys Supervisor must
evaluate the current intake assessment to determine if new intake assessment is required. As a general rule, intake
assessments are valid for one (1) for program transfers. If the intake assessment is older than one (1) year, it is
generally best practice to complete a new intake assessment. The New Journeys Program Supervisor will be
responsible to evaluating the intake assessment and making this determination.

86
Washington State New Journeys Manual – September 2023
APPENDIX D: EXAMPLE COMMUNITY PRESENTATION
A PowerPoint version of this document, with talking points, is available for team use and can be requested from the UW
Program Director Trainer.
GRAYS HARBOR
COUNTY
New Journeys- {Insert regions served}
{Insert name of agency}
Space for agency logo
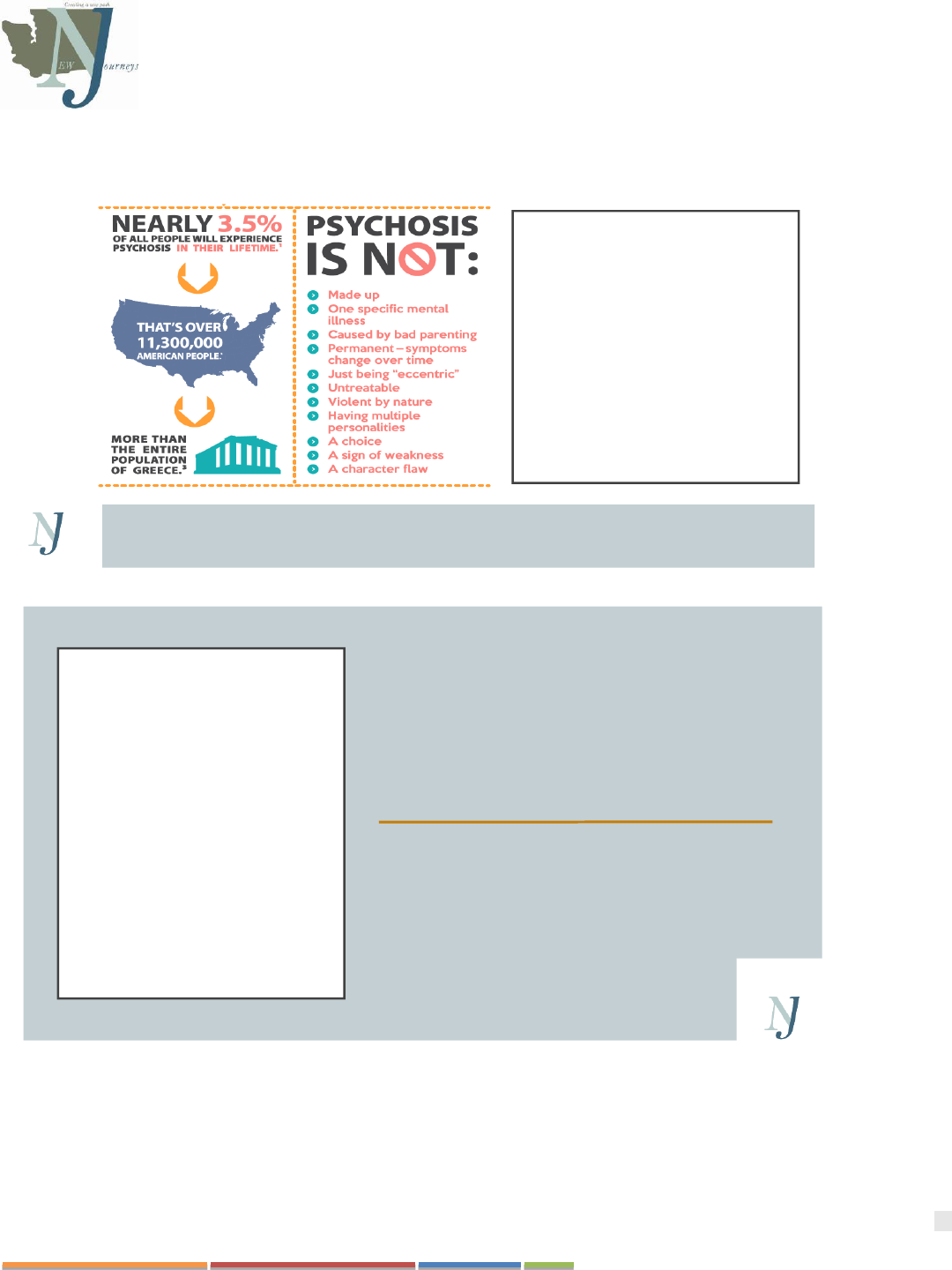
87
Washington State New Journeys Manual – September 2023
WHAT IS FIRST-EPISODE PSYCHOSIS (FEP)?
DESCRIBES CONDITION S
THAT AFFECT TH E MIND,
CAUSING A L O S S O F
C O N TACT W I TH
RE A L I T Y OR TROUBLE
DECIDING ON WHAT IS
REAL AND WHAT IS NOT
REAL.
( P S Y C H O S I S I S A C L U S T E R O F S Y M P T O M S
N OT A D I A G N O S I S . )
THE FACTS
3 OUT OF EVERY 100 YOUNG PEOPLE
WILL EXPERIENCE AN EPISODE OF
PSYCHOSIS IN THEIR LIFETIME, MAKING
IT THE 3
RD
MOST DISABLING CONDITION
IN THE WORLD
THE AVERAGE DURATION OF UNTREATED
PSYCHOSIS IN THE U.S. IS MORE THAN 2
YEARS.
UNTREATED PSYCHOSIS CAN LEAD TO:
• INCREASED SUBSTANCE USE
• MORE HOSPITAL VISITS
• LEGAL TROUBLE
• RISK OF HOMELESSNESS
• PREMATURE DEATH
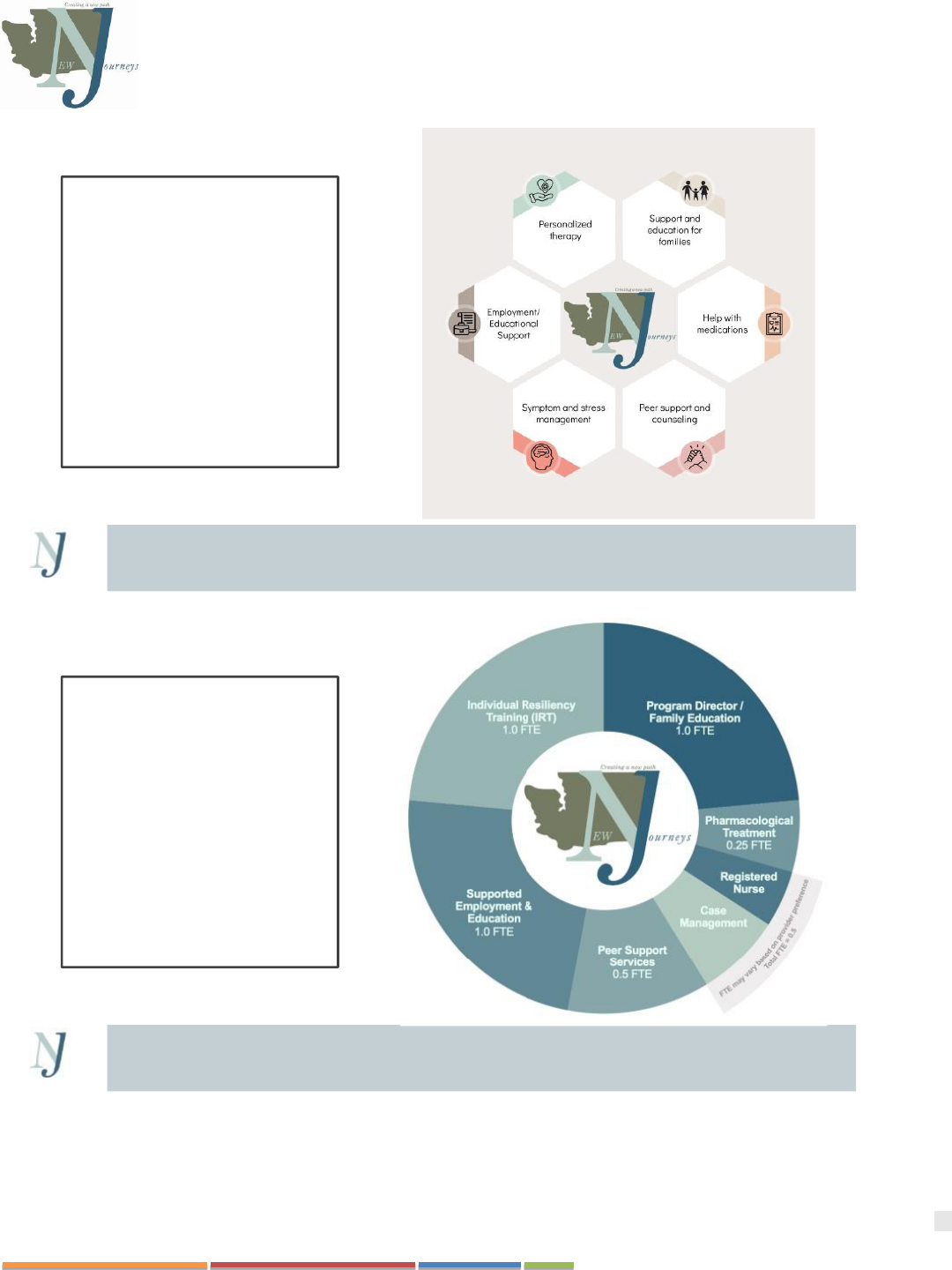
88
Washington State New Journeys Manual – September 2023
89
Washington State New Journeys Manual – September 2023
FAMILY EDUCATION
• Teaching families about psychosis and its treatment
• Help the family process the episode of psychosis
• Reducing relapses by encouraging medication adherence and
monitoring early warning signs of relapse
•
• Reducing family stress through improved communication and problem
solving skills
INDIVIDUAL RESILIENCY
TRAINING
• Processing the experience of psychosis and teaching coping skills
• Teaching social and resiliency skills
• Helping clients achieve personal goals by teaching them about their
disorder and its treatment
• Reducing self-stigmatizing beliefs
90
Washington State New Journeys Manual – September 2023
MEDICATION MANAGEMENT
• Education and assistance in choosing the right medication for symptom
management
• Guidance in managing side effects of management
• Delivery of injectable medications
91
Washington State New Journeys Manual – September 2023
PEER SUPPORT
•
goals
• Disclose personal experiences as appropriate to assist an individual in
their own recovery process.
• Spend time the community to build confidence in abilities and practice
skills alongside participants
• Learn together and from each-others experiences and progress
92
Washington State New Journeys Manual – September 2023
Admission Criteria
1. AGE: 15-40
2. RESIDENT OF: {INSERT COUNTIES SERVED)
3. PSYCHOTIC SYMPTOMS HAVE BEEN
PRESENT BETWEEN 1 WEEK AND 2 YEARS
4. PRIMARY DX OF ONE OF THE FOLLOWING:
• SCHIZOPHRE NIA
• SCHIZOA FFECTIV E DISORDE R
• SCHIZOPHRE NIFORM D ISORDE R
• BRIEF PSYCHOTIC DISORD ER
• DELUSIO NAL DISO RDE R
• OTHER SPECIFIED PSYC HOTIC DISOR DER
All insurances are accepted as well as unfunded
PSYCHOSIS IS NOT KNOWN TO BE
CAUSED BY ONE OF THE FOLLOWING:
• A CURRENT DX OF:
• MOO D DISOR DER
• PERVASIVE DEVE LOPM E NTAL DISOR DER
• AUTISM SPECTRU M DISOR DER
• DOCU MEN TED IQ LESS THA N 7 0
• SUBSTANCE INTOXICATION AND/OR
WITHDRAWAL
• A MEDICAL CONDITION
ACCESS TO
SERVICES
REQUEST IN FO RMAT I ON
CONSULTAT ION ON A CA S E
MAK E A R EFERR AL
CONTACT: PROGRAM DIRECTOR NAME
NEW JOURNEYS CLINICAL SUPERVISOR
CALL:
FAX:
EMAIL:
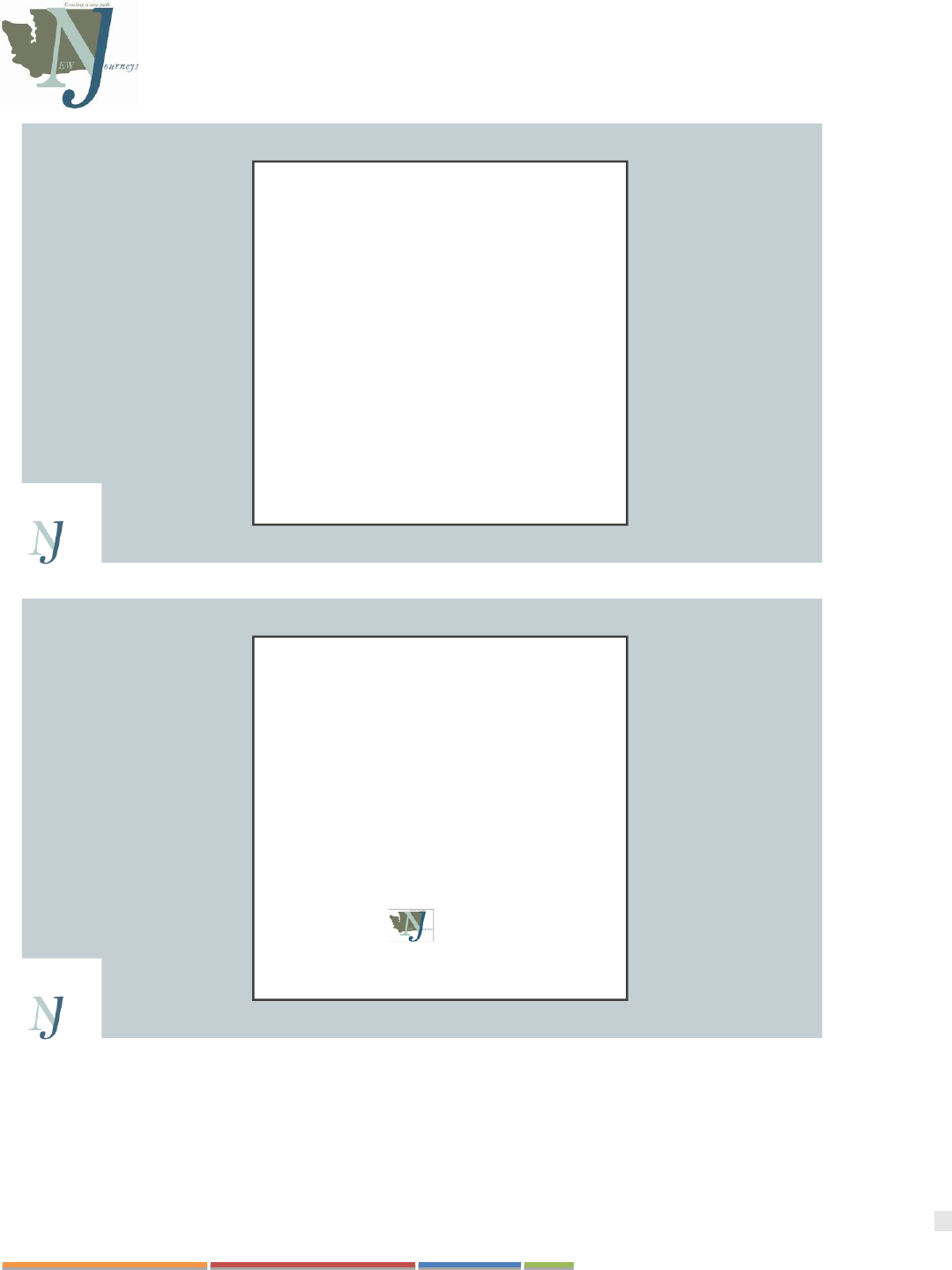
93
Washington State New Journeys Manual – September 2023
QUESTIONS?
THANK YOU!
Name, Credentials
New Journeys Program Supervisor
Contact information
Contact:
Insert agency logo
94
Washington State New Journeys Manual – September 2023
APPENDIX E: NEW JOURNEYS REFERRAL FORM
New Journeys Referral Form
Referral Date: Click or tap to enter a date.
Is the individual aware of the referral? ☐Yes ☐ No
Referred by: Click or tap here to enter text.
Agency/Relationship to individual being referred: Click or tap here
to enter text.
Referent Phone #:
Click or tap here to enter text.
What kind of insurance does the youth/young adult have:
☐Medicaid ☐ Private Insurance Click here to enter text. ☐ No Insurance
Name of referred individual: Click or tap here to enter text.
DOB Click or tap here to enter text.
Identified Gender: Click or tap here to enter text.
Preferred Pronouns: Click or tap here to enter text.
Resident of ☐ {Team inserts county/regions served}
Address:
Click or tap here to enter text.
Phone: Click or tap here to enter
text.
Name/phone # of parent/primary care giver if applicable: Click or tap here to enter text.
Race/ethnicity: Click or tap here to enter text.
Hispanic origin? ☐ Yes ☐ No
Highest grade level completed:
Click or tap here to enter text.
School: Click or tap here to enter
text.
Does the referred individual have an existing mental health diagnosis? ☐ Yes ☐ No
Please list any known diagnoses: Click or tap here to enter text.
Is the individual already receiving services for mental health? ☐ Yes ☐ No
If yes, where? Click or tap here to enter text.
Reason for Referral: Click or tap here to enter text.
Please review the following items and check all that apply:
☐ The individual’s speech doesn’t make sense
☐ The individual has behaviors, speech, or beliefs are uncharacteristic and/or bizarre
☐ The individual reports hearing voices or sounds that others do not
☐ The individual feels that other people are putting thoughts in their head, stealing their thoughts
☐ The individual believes others can read their mind (or vice versa)
☐ The individual believes that they do not exist or that their surroundings are not real
95
Washington State New Journeys Manual – September 2023
☐ The individual has experienced a significant decline overall functioning
☐ The individual has experienced significant changes in sleep (sleeping less or sleeping too much)
☐ The individual has been experiencing increased fear or anxiety for no apparent reason
☐ There is a family history of major psychotic disorder
☐ The individual has an existing diagnosis of autism spectrum disorder
☐ The individual has a history of Drug/marijuana/alcohol use (list substances used below):
Click or tap here to enter text.
Is the individual experiencing any other symptoms not listed? ☐ Yes ☐ No
Please explain: Click or tap here to enter text.
When did you first notice these changes in the individual being referred? Click or tap here to enter text.
Safety Concerns? Click or tap here to enter text.
Has the individual ever been prescribed antipsychotic medication? ☐ Yes ☐ No
What medications are currently being prescribed? Click or tap here to enter text.
Who is prescribing the medications? Click or tap here to enter text.
Submit form to: {Insert name of Program Director}, New Journeys Program Director
Fax: {Insert Fax #}
Email: {Insert Phone #}
Questions? Call {Insert name of PD and phone #}

96
Washington State New Journeys Manual – September 2023
APPENDIX F: WEEKLY TEAM MEETING PARTICIPANT TRACKING SHEET
Participant
Goals
Psychiatric Care
Provider notes
IRT Specialist notes
Family Education
Specialist notes
SEE Specialist notes
Peer Specialist
notes
Andy
(1) paid
employment; (2)
improved
connection with
others, including
two new friends;
and (3) improve
health by decreasing
BMI to <30
Past week: He is
currently on
risperidone but
continues to be
bothered by weight
gain and is sedated;
On propranolol and
takes Melatonin PRN
for sleep.
Plan:
Start to cross-taper to
Abilify.
Past week:
Working on Having
Fun & Developing
Good Relationships
module.
Plan:
Continue with
Nutrition & Exercise
module. Work with
Peer to walk around
Green Lake and make
eye contact with three
people. Will discuss
possible family
meeting.
Past week:
Contacted mom to
resume weekly
sessions.
Plan:
Will connect with local
support groups and
resources. Will initiate
family meeting after
IRT discusses with
Andy.
Past week: No contact
with Andy over the
past week, per his
request.
Plan:
Will re-approach likes
and dislikes related to
recent job loss, pros
and cons of disclosure
at the workplace,
availability of supports
to better assure
satisfaction and success
in employment
Past week:
Has not engaged with
Peer so far.
Plan:
Will use strategies for
engagement, including
motivational interviewing
and sharing aspects of
lived experiences. Will
engage with walks
around Green Lake and
discuss bus routes. Will
also talk about pros and
cons of disclosure at
work, sharing lived
experiences regarding
asking for
accommodations.
97
Washington State New Journeys Manual – September 2023
Participant
Goals
Psychiatric Care
Provider notes
IRT Specialist notes
Family Education
Specialist notes
SEE Specialist notes
Peer Specialist
notes
Megan
Return to school
Past week: On
discharge meds of
risperidone 2 mg. Met
with Megan alone and
with mother. Hesitant
to increase dose.
Introduced possibility
of LAI.
Plan: Continue current
dose and have Megan
and mother track
functioning and side
effects. Have them
review LAI video
before doing
decisional balance
worksheet.
Past week: No
contact yet.
Plan: Orient Megan
to IRT. Elicit
commitment to
meeting weekly and
establish their
preference for
meeting place.
Past week: Met with
mom and Megan to
orient to New
Journeys.
Plan: Will begin
weekly sessions with
mom starting with
“Just the Facts”
modules in the
NAVIGATE Family
Education Manual.
Past week: Engaged
with Megan, shared
nature and benefits of
SEE services. Early
interest appears to be
focused on a return to
school asap. Agreed to
keep talking.
Plan: Continue
engagement, offer to
assist in development
of plan to return to
school, begin gathering
information for the
educational profile,
open up the topic of
disclosure and related
accommodations.
Past week: Shared lived
experience and explained
role. Shared info
regarding possible open
mic nights in the area.
Plan: Scheduled next
meeting to check out a
comedy open mic at a
local community college
that they are interested in
performing at.

98
Washington State New Journeys Manual – September 2023
APPENDIX G: NETWORK CONTACTS
